Healthcare Organizations & Transactions
![]() Institute
for the Study of
Institute
for the Study of ![]()
Healthcare Organizations & Transactions
Hypnosis in Surgery:
Efficacy, Specificity, and Utility
John
F. Kihlstrom
University
of California, Berkeley
Paper presented at the annual meeting of the American Psychological Association, San Francisco, August 2001. The point of view represented in this paper is based on research supported by Grant MH-35856 from the National Institute of Mental Health. I thank Lucy Canter Kihlstrom for her comments during the preparation of this paper.
No phenomenon of hypnosis is more dramatic than analgesia, and none has more potential for clinical application. Nevertheless, hypnosis has had a hard time taking its rightful place in the standard of care for patients in pain (Kihlstrom, 2000).
What are the Origins of Surgical Hypnosis?
 Think back to the
1840s, before hypnosis even had its proper name, and was still
called "animal magnetism" or even "mesmerism". Up to this time,
medical and dental surgery was performed without anesthetic, for
the simple reason that anesthetics were unavailable ( see also
Fenster, 2001; Keys, 1963; Rushman, Davies, & Atkinson,
1996). The situation in the early 19th century was
aptly summarized by Oliver Wendell Holmes, the great American
physician and jurist, with the comment that nature offers only
three natural anesthetics: sleep, fainting, and death. Patients
may have been given alcohol or laudanum to dull the senses, but
these treatments often made them more, not less, difficult to
manage. Mostly, patients were just strapped to the operating
table and had to "bite the bullet" -- a situation vividly
portrayed by the English novelist Fanny Burney in her memoir of
her own mastectomy, performed in 1810. Robert Liston, Britain's
most famous and accomplished surgeon, even scolded a patient for
lacking "discipline" during surgery, and threatened to terminate
the procedure unfinished.
Think back to the
1840s, before hypnosis even had its proper name, and was still
called "animal magnetism" or even "mesmerism". Up to this time,
medical and dental surgery was performed without anesthetic, for
the simple reason that anesthetics were unavailable ( see also
Fenster, 2001; Keys, 1963; Rushman, Davies, & Atkinson,
1996). The situation in the early 19th century was
aptly summarized by Oliver Wendell Holmes, the great American
physician and jurist, with the comment that nature offers only
three natural anesthetics: sleep, fainting, and death. Patients
may have been given alcohol or laudanum to dull the senses, but
these treatments often made them more, not less, difficult to
manage. Mostly, patients were just strapped to the operating
table and had to "bite the bullet" -- a situation vividly
portrayed by the English novelist Fanny Burney in her memoir of
her own mastectomy, performed in 1810. Robert Liston, Britain's
most famous and accomplished surgeon, even scolded a patient for
lacking "discipline" during surgery, and threatened to terminate
the procedure unfinished.
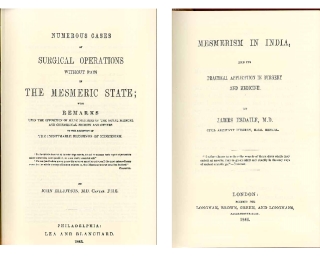 Against this
background, it was little short of amazing when John Elliotson,
the revered Professor of Practical Medicine at University
College, London, and his protege James Esdaile, a medical
officer for the British East India Company, each reported a
large number of surgeries performed painlessly, with the
mesmeric trance as the only anesthetic agent. Against the
suspicion of deceit and self-delusion, Esdaile noted the simple
fact that his patients referred their family and friends to his
service. But he also had data of a harder kind: at a time when
surgical mortality was about 40%, Esdaile's death rate was
reduced to only about 5% -- an objective outcome that he
plausibly attributed to the successful relief of pain with
mesmerism.
Against this
background, it was little short of amazing when John Elliotson,
the revered Professor of Practical Medicine at University
College, London, and his protege James Esdaile, a medical
officer for the British East India Company, each reported a
large number of surgeries performed painlessly, with the
mesmeric trance as the only anesthetic agent. Against the
suspicion of deceit and self-delusion, Esdaile noted the simple
fact that his patients referred their family and friends to his
service. But he also had data of a harder kind: at a time when
surgical mortality was about 40%, Esdaile's death rate was
reduced to only about 5% -- an objective outcome that he
plausibly attributed to the successful relief of pain with
mesmerism.
 Like
Elliotson, Esdaile hoped that the new technique would become
widely available for the benefit of the public, but he also
expressed the fear "that not many of this generation will live
to benefit by Mesmerism, if they wait till it is admitted into
the Pharmacopoeia". And he was right. On October 18, 1846,
before Esdaile's book could even be published, William T.G.
Morton, a Boston dentist, placed an inhaler containing an
ether-soaked sponge to the face of the patient Gilbert Abbot.
The Harvard surgeon John Collins Warren, who himself had
experimented unsuccessfully with mesmeric anesthesia earlier in
his career, then removed a tumor from Abbott's neck without the
patient showing any awareness or signs of pain.
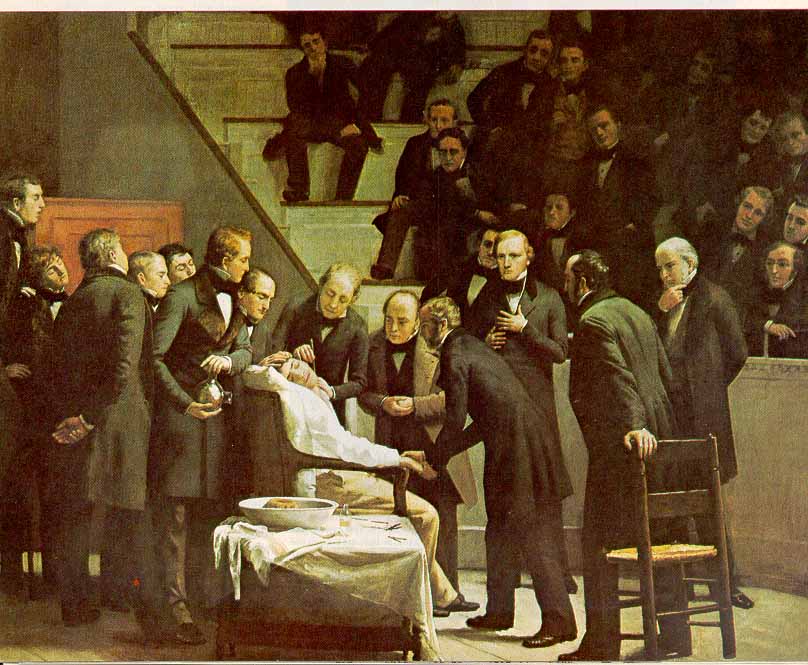
Like
Elliotson, Esdaile hoped that the new technique would become
widely available for the benefit of the public, but he also
expressed the fear "that not many of this generation will live
to benefit by Mesmerism, if they wait till it is admitted into
the Pharmacopoeia". And he was right. On October 18, 1846,
before Esdaile's book could even be published, William T.G.
Morton, a Boston dentist, placed an inhaler containing an
ether-soaked sponge to the face of the patient Gilbert Abbot.
The Harvard surgeon John Collins Warren, who himself had
experimented unsuccessfully with mesmeric anesthesia earlier in
his career, then removed a tumor from Abbott's neck without the
patient showing any awareness or signs of pain.
The news traveled fast: Morton's success was duplicated in Paris on December 15, and in London on December 19. On December 21, after another success, Robert Liston proclaimed
"This Yankee dodge, gentlemen, beats mesmerism hollow".
Within two years, ether, nitrous oxide, chloroform, and other chemical anesthetics were widely used in dentistry, surgery, and obstetrics. Even Queen Victoria bore her last child, Prince Leopold, under chloroform. Surgery finally had an anesthetic technique that was, in the words of Henry J. Bigelow's authoritative report of four cases performed by Morton, "inevitable, complete, and safe"; and as an approved medical technique, mesmerism was consigned to the dustbin of history.
For the next hundred years or so, hypnosis survived mostly as a topic of laboratory investigation, and found little application in the clinic outside psychotherapy. Robert Sears and Frank Pattie performed pioneering studies of hypnotic analgesia and tactile anesthesia in the 1930s, but there were a few other experimental studies, and even fewer performed in clinical settings (Weitzenhoffer, 1953). In the meantime, advances in antiseptic practice and asepsis, regional and local anesthesia, the synthesis of nontoxic and nonaddictive substitutes for cocaine and morphine, and the introduction of muscle relaxation and artificial respiration by means of a tracheal tube, all made chemical anesthesia and analgesia increasingly "inevitable, complete, and safe". These developments must have further reduced interest in hypnosis.
When Did Hypnosis Re-Enter Surgical Practice?
Still, hypnosis gradually crept back into medical practice -- perhaps aided by its successful use in World War II, when chemical analgesics and anesthetics were not always available for the treatment of the wounded. When Jack and Josephine Hilgard surveyed the literature their review of Hypnosis in the Relief of Pain (Hilgard & Hilgard, 1975), they listed more than two dozen cases, published between 1955 and 1974, in which hypnosis had been used as the sole analgesic or anesthetic agent in surgery. But dramatic as these case reports were, the general consensus in the field was that no more than 10% of unselected patients, and probably far fewer, could tolerate such invasive procedures with hypnosis alone. Far more important, in my view, was the publication of several extensive case series, not just individual case studies, of hypnosis for clinical pain. Chief among these were Ralph August's report of 1000 consecutive obstetrical cases and Cangello's study of cancer pain, both published in 1961, and Davidson's favorable comparison of hypnosis to natural childbirth, published in 1962.
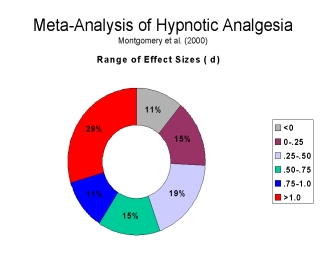 Based on their
review, the Hilgards estimated that approximately half of an
unselected patient population could obtain significant pain
relief, defined as a one-third reduction in felt pain, from
hypnosis alone. Recently, a quantitative review by Guy
Montgomery and his colleagues has confirmed this conclusion
(Montgomery, DuHamel, & Redd, 2000). The effect of hypnosis
on pain is moderately large, even when there has been no
selection for hypnotizability. Equally important, in the present
context, the effect of hypnosis is even greater in the clinic
than in the laboratory.
Based on their
review, the Hilgards estimated that approximately half of an
unselected patient population could obtain significant pain
relief, defined as a one-third reduction in felt pain, from
hypnosis alone. Recently, a quantitative review by Guy
Montgomery and his colleagues has confirmed this conclusion
(Montgomery, DuHamel, & Redd, 2000). The effect of hypnosis
on pain is moderately large, even when there has been no
selection for hypnotizability. Equally important, in the present
context, the effect of hypnosis is even greater in the clinic
than in the laboratory.
Especially given the risks to the fetus from halogenated ethers and narcotics administered to women in parturition, and the risks to cancer patients from chronic narcotic use, you would have thought that hypnosis would be a natural alternative for these kinds of patients. Nevertheless, in the succeeding quarter century, relatively few clinical studies were published, and hypnosis pretty much dropped out of the physician's armamentarium. In retrospect, we can identify at least three reasons for this turn of events.
In the first place, hypnotic analgesia is safe, but it is neither inevitable nor complete, to use Bigelow's terms. There are individual differences in response to hypnotic analgesia, just as there are to other hypnotic suggestions; and so the majority of patients who try hypnosis alone are still going to feel some pain. Chemical analgesia and anesthesia is the standard of care precisely because it is more reliable -- more inevitable, more complete -- than hypnosis.
Second, hypnosis was overtaken by new developments in anesthetic technique and medical practice. In obstetrics, for example, Caesarian section became increasingly popular among doctors, while epidural anesthesia became increasingly popular among women. The technique of conscious sedation, now extremely popular for outpatient surgery and other office procedures, allows the patient to remain awake and interact with the medical team while minimizing discomfort during the procedure and inducing amnesia for it afterward. Patient-controlled analgesia, during and after procedures, also allows patients to remain awake while enhancing their feelings of control. These are precisely the reasons to use hypnosis, but if physicians can obtain the same effects more reliably with drugs, they're naturally going to turn to drugs.
Third, during the
1950s, just at the time that hypnosis was re-emerging in
medicine, the standards for clinical research changed. Henry K.
Beecher began writing about the placebo effect (e.g., Beecher,
1955), while Walter Modell wrote about the importance of
randomization and controlled comparisons between treatments
(e.g., Modell & Houde, 1958). It was no longer sufficient to
document a new technique by presenting a case or two in
anecdotal fashion, or even a large consecutive series of cases,
and have other practitioners adopt it for themselves. In the
current healthcare environment, in which "evidence-based
medicine" is firmly established (and incidentally raising the
question of just what kind of medicine we used to have),
the gold standard of proof for clinical interventions involves
randomized clinical trials against control groups that receive
placebos, or the current standard of care. The sad fact is that
there haven't been many such studies -- at least until recently.
Does Hypnosis Really Work for Surgical Pain?
In this respect, I attach particular importance to the work of Elvira Lang and her colleagues, who have provided the most compelling demonstrations of the clinical efficacy of hypnotic analgesia. In these studies, patients who have been scheduled for a variety of invasive diagnostic and therapeutic procedures, have been randomly assigned to one of two conditions: patient-controlled conscious sedation, usually with a combination of Midazolam and Fentanyl, which is the standard of care; and conscious sedation plus a hypnotic intervention involving relaxation and counterpain imagery.
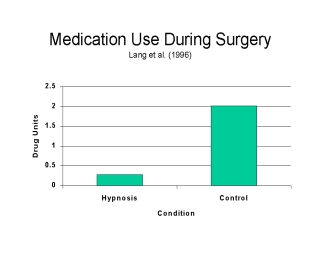 The first of these
studies, published in 1996, was a small-scale study, with 30
patients randomized to hypnotic and non-hypnotic treatment
groups (Lang, Joyce, Spiegel, Hamilton, & Lee, 1996).
Only 4 of 16 patients in the hypnotic condition, compared to 13
of 14 patients in the control condition, requested medication
during the procedure. The hypnotic patients also received fewer
drug units than controls.
The first of these
studies, published in 1996, was a small-scale study, with 30
patients randomized to hypnotic and non-hypnotic treatment
groups (Lang, Joyce, Spiegel, Hamilton, & Lee, 1996).
Only 4 of 16 patients in the hypnotic condition, compared to 13
of 14 patients in the control condition, requested medication
during the procedure. The hypnotic patients also received fewer
drug units than controls.
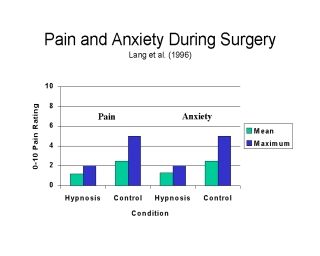 Nevertheless, the
hypnotized patients experienced less pain and less anxiety than
the controls.
Nevertheless, the
hypnotized patients experienced less pain and less anxiety than
the controls.
 Interestingly,
there were also fewer procedural interruptions due to
hemodynamic instability. On every outcome variable examined, the
hypnotic group was at an advantage. Unfortunately, the sample
sizes in this study were too small to yield statistically
significant results for the pain and anxiety ratings.
Interestingly,
there were also fewer procedural interruptions due to
hemodynamic instability. On every outcome variable examined, the
hypnotic group was at an advantage. Unfortunately, the sample
sizes in this study were too small to yield statistically
significant results for the pain and anxiety ratings.
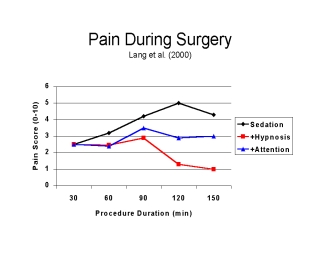 Fortunately,
Fortunately, 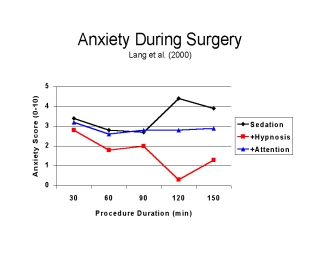 however, last year
Lang reported a larger-scale study, with 241 patients randomized
to three groups (Lang et al., 2000). In this research, all
patients received standard patient-controlled conscious
sedation; one-third received a standardized hypnosis treatment
as well, one-third a structured attention manipulation, and the
remainder were controls. In this case, the addition of
hypnosis afforded significantly greater pain relief than
conscious sedation alone, especially in the latter half of the
procedure. Hypnosis also significantly decreased
anxiety.
however, last year
Lang reported a larger-scale study, with 241 patients randomized
to three groups (Lang et al., 2000). In this research, all
patients received standard patient-controlled conscious
sedation; one-third received a standardized hypnosis treatment
as well, one-third a structured attention manipulation, and the
remainder were controls. In this case, the addition of
hypnosis afforded significantly greater pain relief than
conscious sedation alone, especially in the latter half of the
procedure. Hypnosis also significantly decreased
anxiety.
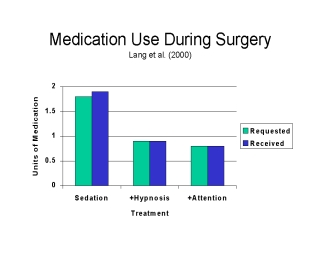 The hypnotic group
requested, and received, less medication than the controls.
The hypnotic group
requested, and received, less medication than the controls.
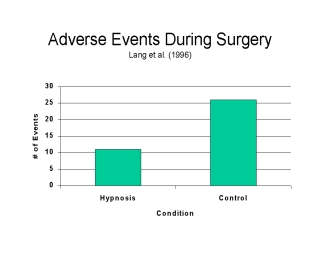
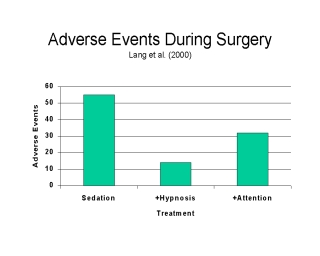 There
There 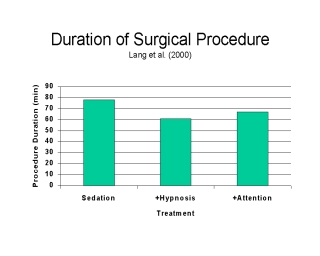 were fewer adverse
events with hypnosis, and so the procedures took less time
on average. On every variable, hypnosis was superior to the
attentional manipulation, so hypnosis is not only efficacious;
the effects are also specific to hypnosis.
were fewer adverse
events with hypnosis, and so the procedures took less time
on average. On every variable, hypnosis was superior to the
attentional manipulation, so hypnosis is not only efficacious;
the effects are also specific to hypnosis.
These two studies, taken together, satisfy all but one of the Division 12 criteria for a "well-established" treatment (Chambless & Ollendick, 2001): there are two between-group experiments in which adjunctive hypnosis proved superior to the standard treatment; the hypnotic procedure is clearly described; and the characteristics of the samples are specified. The only remaining criterion is that the effects be demonstrated by at least two different investigators or teams. Actually, that criterion had already been fulfilled by the earlier generation of clinical studies, of the sort reviewed by the Hilgards. But in fact, there is also a series of studies by a group of Belgian investigators, using what they call "hypnosedation" as an adjunct to conscious sedation (Faymonville, Meurisse, & Fissette, 1999).
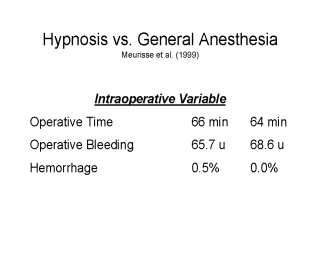 One
One 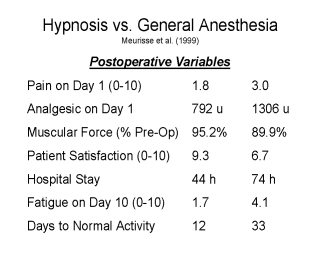 study, for
example, compared 218 cases of endocrine surgery performed under
hypnosedation with 121 closely matched cases performed under
general anesthesia (Meurisse et al., 1999). Interestingly, fewer
than 1% of the patients in the hypnosis group required
conversion to general anesthesia, requiring only local
anesthetic and minimal sedation -- which provides prima
facie evidence for the effectiveness of
hypnosis. In terms of intra-operative outcomes --
operative time, bleeding, etc. -- the two groups were
indistinguishable. But all the measures of postoperative
outcome significantly favored hypnosis: less pain and analgesic
medication on the first recovery day, greater muscle strength,
lower postoperative fatigue, shorter hospital stay, quicker
return to normal activity, and greater patient satisfaction.
study, for
example, compared 218 cases of endocrine surgery performed under
hypnosedation with 121 closely matched cases performed under
general anesthesia (Meurisse et al., 1999). Interestingly, fewer
than 1% of the patients in the hypnosis group required
conversion to general anesthesia, requiring only local
anesthetic and minimal sedation -- which provides prima
facie evidence for the effectiveness of
hypnosis. In terms of intra-operative outcomes --
operative time, bleeding, etc. -- the two groups were
indistinguishable. But all the measures of postoperative
outcome significantly favored hypnosis: less pain and analgesic
medication on the first recovery day, greater muscle strength,
lower postoperative fatigue, shorter hospital stay, quicker
return to normal activity, and greater patient satisfaction.
Unfortunately, the Belgian studies did not involve random assignment, but I think this should not be held against them. The principles of informed consent make randomization very difficult to achieve, and in any event there was no preselection of patients for hypnotizability, which is surely the most important potential source of bias. That is why the Lang studies, which do involve randomization, are so important. Without them, hypnosis would have to be classified merely as "probably efficacious". Still, we could use more randomized studies, employing different kinds of surgical procedures and different diagnostic related groups, to clinch the case that hypnotic analgesia meets the fourth and final criterion as a specific and efficacious technique for the relief of clinical pain. But this "proof" has to be qualified: there is no methodologically acceptable evidence that hypnosis, all by itself, can substitute for the chemical analgesia and anesthesia that is the standard of care. Hypnosis is not an alternative to traditional medicine, but it is an effective complement to chemical anesthesia.
This should be a good time for hypnosis: under the rubric of "complementary", or "alternative", medicine (CAM), healthcare consumers are seeking alternatives to the chemical and surgical interventions that are the standard of care in modern scientific medicine; healthcare professionals are increasingly open to these alternatives; health plans are, tentatively, willing to pay for them; and the National Institutes of Health are seriously interested in evaluating them. This creates an atmosphere in which hypnosis can re-enter clinical practice.
One issue that has to be confronted is the relationship between hypnosis and placebo. The placebo effect has become the "jewel in the crown" of complementary and alternative medicine -- the most powerful, most convincing demonstration of the effect of the mind on the body. But hypnosis can have similar effects, leading some prominent authorities to identify hypnosis as a kind of placebo effect itself (e.g., Kirsch, 1994). I think this position is wrong on the merits -- the classic study by McGlashan, Evans, and Orne shows clearly that hypnotic analgesia is not mediated by placebo, though hypnosis, like every active treatment, has a placebo component (McGlashan, Evans, & Orne, 1969). But I understand and sympathize with the motive, which is to further "domesticate" hypnosis by linking it to a psychosocial treatment that (almost) everyone agrees is powerful.
Still and all, I think that any linkage between hypnosis and placebo is bound to backfire, for reasons that have to do with what can be described, fairly and without irony, as the biologization of medicine. The last 50 years have worked a revolution in how physicians perceive themselves and their work. Surgeons no longer want to cut off diseased body parts; they want to repair or replace damaged tissues and organs. Internists don't want to palliate symptoms; they want to correct underlying disease processes. For all the lip service being paid to the importance of psychosocial variables, mainstream medicine construes placebo effects as nuisances to be minimized, not as psychological phenomena to be put to use. Put bluntly, doctors don't want to give their patients placebos. They want to cure disease. Any suspicion that hypnosis is "just" a placebo is going to make most mainstream physicians avoid it like the plague. That's why I think that hypnosis has much to gain by presenting itself as a complement, rather than as an alternative, to traditional medicine. It is the addition of hypnosis, to standard treatments, that confers many benefits. It is as an adjuvant treatment that hypnosis will re-establish itself in the clinic.
But now we meet a new challenge. Healthcare professionals don't just work in an environment of evidence-based medicine. They also work in an environment of managed care. And whenever I tell practitioners about these new studies, their first question is whether hypnosis is reimbursable by managed care. Love it or hate it, managed care is here to stay, and managed care won't pay for a treatment that isn't effective -- why should it? But managed care also won't pay for a treatment that is not cost-effective as well. While some health plans will now pay for complementary treatments, this policy will not last long unless those treatments prove cost-effective as well as effective.
Fortunately, here again we already have evidence about the utility of hypnosis, above and beyond its efficacy and specificity. Both Lang's studies and those of the Belgian group clearly indicate that when hypnosis is used as an adjunct to conscious sedation, patients use fewer medications and experience fewer complications, procedures take less time, and discharge comes sooner. This is prima facie evidence that hypnosis saves money at the same time as it improves the quality of care -- a dynamite combination from the perspective of any managed-care organization.
Of course, you have to factor in the cost of the hypnotist. But note that in both series of studies hypnosis is given to everyone, regardless of hypnotizability, so there is no expense for patient screening. And there is nothing about the hypnotic intervention that can't be done by anesthetists, including nurse anesthetists, as part of their regular duties. So the extra expense incurred by adjuvant hypnosis strikes me as minimal. In fact, at a recent conference Lang and Rosen reported a cost analysis of their 2000 study projecting a savings of $338 per case with hypnosis, if the anesthetist does the hypnosis, and $290 per case if an additional staff member does the job (Lang & Rosen, 1999). A couple hundred dollars here, and a couple hundred dollars there, spread over the thousands of patients who receive local and regional anesthesia or conscious sedation every year, and pretty soon you're talking about real money.
Partly as a reaction to managed care, there has arisen another movement in healthcare, towards quality of care. People want to save money, but they don't want to sacrifice quality of service. But what do we mean by "quality"? At the lowest common denominator, we can say that people are getting quality of care if they're receiving the standard of care. By that standard, if hypnosis improves the efficacy of standard drug treatment, then hypnosis improves the quality of care almost by definition. But we mean more than that by "quality": we mean, for example, that people should be satisfied with the way the treatment was delivered, not just its outcome.
Again, the studies I've reviewed here suggest that hypnosis improves the quality of anesthesia services, not just their efficacy and cost-effectiveness. Patients gain an increase in perceived self-control; there are fewer intra-operative complications; there is reduced post-operative pain and fatigue, and there is a faster return to normal activities. It is therefore not surprising that, in the Belgian studies, the addition of hypnosis leads to increased patient satisfaction.
Based on the literature I've reviewed here and elsewhere (Kihlstrom, 2000), adjuvant hypnosis appears to pass four important tests: It is effective, in that drugs plus hypnosis yield more pain relief than drugs alone. As a clinical practice, it rests on a firm scientific base that shows, among other things, that it is a specific treatment, different from both placebo and from other psychosocial interventions. It is cost effective, reducing the cost of procedures by a nontrivial sum. And it improves the quality of care. A few more studies like these, and hypnosis will no longer be an adjuvant to conventional treatment. It will be the new standard of care. And at that point, more than 150 years later, we will finally reverse the verdict of Robert Liston:
Drugs plus hypnosis, people, beat drugs alone hollow!
Beecher, H. K. (1955). The powerful placebo. Journal of the American Medical Association, 159, 1602-1606.
Chambless, D. L., & Ollendick, t. H. (2001). Empirically supported psychological interventions: Controversies and evidence. Annual Review of Psychology, 52, 685-716.
Faymonville, M. E., Meurisse, M., & Fissette, J. (1999). Hypnosedation: A valuable alternative to traditional anaesthetic techniques. ACTA CHIRURGICA BELGICA, 99(4), 141-146.
Fenster, J. M. (2001). Ether Day: The strange tale of America's greatest medical discovery and the haunted men wo made it. New York: HarperCollins.
Hilgard, E. R., & Hilgard, J. R. (1975). Hypnosis in the relief of pain. Los Altos, Ca.: Kaufman.
Keys, T. E. (1963). Ths history of surgical anesthesia. New York: Dover.
Kihlstrom, J. F. (2000, November 2). Hypnosis and pain: Time for a new look. Paper presented at the Annual meeting of the American Pain Society, Atlanta, Ga.
Kirsch, I. (1994). Clnical hypnosis as a nondeceptive placebo: Empirically derived techniques. American Journal of Clinical Hypnosis, 37, 95-105.
Lang, E. V., Benotsch, E. G., Fick, L. J., Lutgendorf, S., Berbaum, M. L., Berbaum, K. S., Logan, H., & Spiegel, D. (2000). Adjunctive non-pharmacological analgesia for invasive medical procedures: A randomised trial. Lancet, 355(April 29), 1486-1500.
Lang, E. V., Joyce, J. S., Spiegel, D., Hamilton, D., & Lee, K. K. (1996). Self-hypnotic relaxation during interventional radiological procedures: Effects on pain perception and intravenous drug use. International Journal of Clinical & Experimental Hypnosis, 44, 106-119.
Lang, E. V., & Rosen, M. P. (1999). Impact of adjunct self-hypnotic relaxation on cost of IV conscious sedation during outpatient angiography: A decision analysis model. RADIOLOGY, 213P, 434.
McGlashan, T. H., Evans, F. J., & Orne, M. T. (1969). The nature of hypnotic analgesia and placebo response to experimental pain. Psychosomatic Medicine, 31, 227-246.
Meurisse, M., Defechereux, T., Hamoir, E., Maweja, S., Marchettini, P., Gollogly, L., Degauque, C., Joris, J., & Faymonville, M. E. (1999). Hypnosis with conscious sedation instead of general anaesthesia? Applications in cervical endocrine surgery. ACTA CHIRURGICA BELGICA, 99(4), 151-158.
Modell, W., & Houde, R.W. (1958). Factors influencing clinical evaluation of drugs. Journal of the American Medical Association, 167, 2190-2198.
Montgomery, G. H., DuHamel, K. N., & Redd, W. H. (2000). A meta-analysis of hypnotically induced analgesia: How effective is hypnosis? International Journal of Clinical and Experimental Hypnosis, 48(2), 138-153.
Rushman, G. B., .Davies, N. J. H., & Atkinson, R. S. (1996). A short history of anaesthesia: The first 150 years. Oxford, U.K.: Butterworth Heinemann.
Weitzenhoffer, A. M.
(1953). Hypnotism: an objective study in suggestibility.
New York: Wiley.