Note: Plenary address presented to the annual
meeting of the Society for Clinical and Experimental
Hypnosis, Berkeley, California, October 4, 2013.
This paper honors Dr. Dabney Ewin,
Clinical Professor of Surgery and Psychiatry at Tulane
University Medical School, whose clinical work using
hypnosis inspired me to take psychosomatics
seriously. Any clinician interested in using
hypnosis in treatment would profit from Dr. Ewin's little
book, 101 Things I Wish I'd Known When I Started Using
Hypnosis (Crown House Publishing, 2009).
Thank you for your kind introduction. It's always a special
privilege to speak before this group.
In fact, this occasion sent my thoughts
reaching back to my very first SCEH meeting, which was my
very first scientific conference. It was 1970, my
first year at graduate school, in Philadelphia: Martin Orne
organized the local arrangements, and Fred Evans was
co-chair (with Erik Wright) of the scientific program. I didn't present
any research -- I had only just begun working with Martin,
and Fred, and Emily Orne, and even though we had results
from our first study of temporal organization during
posthypnotic amnesia, the Scientific Program had been set
long before. But
everybody in Martin's lab was seconded to help out at the
meeting, so I did get to be present for the whole thing.
And what a meeting it was!
The research workshop lasted three whole days. The
scientific program began, as it always did in those days,
with clinical research.
Andre Weitzenhoffer discussed the "hypnotic stare",
and Herb Spiegel introduced his eye-roll sign for
hypnotizability. Robert
W. White, who had been Martin's dissertation advisor,
reflected on the implications of hypnosis for personality,
motivation, and social interaction. Perry London
discussed the prospects for increasing hypnotizability
through EEG alpha training.
There was a symposium on antisocial behavior and
hypnosis. Ted
Barber offered his "new" conceptualization of hypnosis
(which turned out to look awfully like the old one). Throughout it all,
there was Paul Sacerdote and Erika Fromm in the front row
during the research reports, and Jack Hilgard and Ron Shor
in the front row during the clinical papers. Clinicians and
experimentalists together, just as it says in the name of
our Society and the title of our Journal.
 OK, I'll admit it: I had to
look some of those details up.
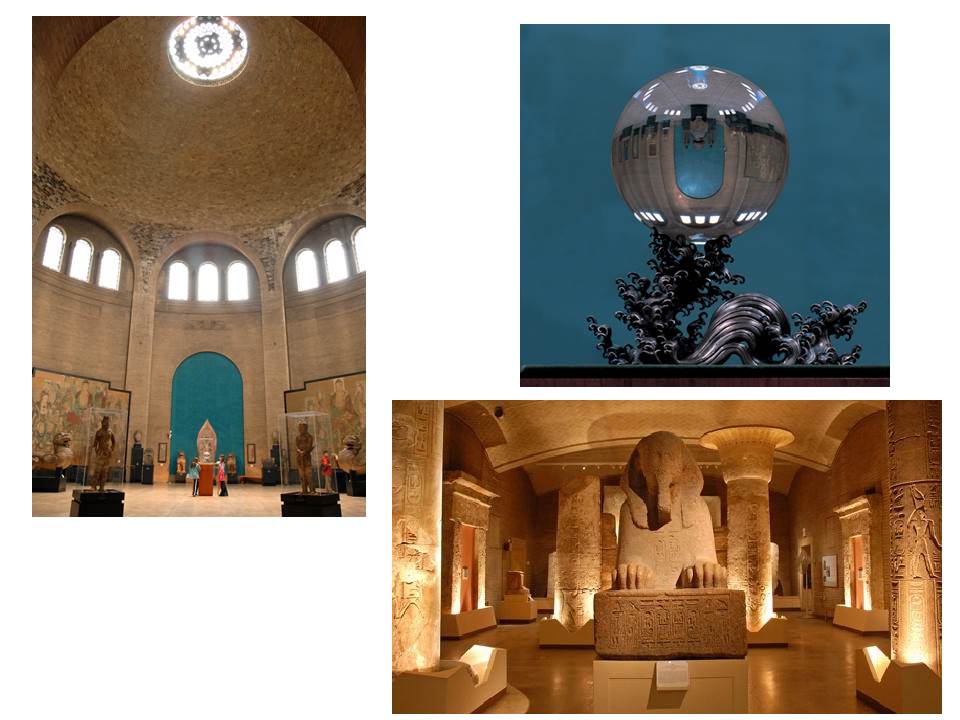
But one memory especially has stuck with me, over all
these years: the Presidential Banquet at the University of
Pennsylvania Museum, one of the best archeological museums in
the world; cocktail hour in the Chinese Rotunda, surrounding
the famous crystal ball, 55 pounds of transparent quartz;
dinner in the Egyptian Room, surrounded by mummies (steaks
grilled on hibachis). Leston
Havens, the great historian of psychiatry, talking about the
connection between hypnosis and hysteria. Did I mention it was
Halloween weekend? Was
that David Rosenhan or Phil Zimbardo dressed in a magician's
cape, cane, and top hat?
I don't remember those details anymore. But what I do
remember was that as soon as the festivities began, the Museum
staff told Martin that the cash bar was strictly illegal: this
was Pennsylvania, and there was no selling alcohol without a
state license. So
the bar had to be closed -- except that Bernard Raginsky
pulled out his checkbook and covered the whole expense. A great metaphor for
the commitment of individual members to the good of the
Society as a whole.
OK, I'll admit it: I had to
look some of those details up.
But one memory especially has stuck with me, over all
these years: the Presidential Banquet at the University of
Pennsylvania Museum, one of the best archeological museums in
the world; cocktail hour in the Chinese Rotunda, surrounding
the famous crystal ball, 55 pounds of transparent quartz;
dinner in the Egyptian Room, surrounded by mummies (steaks
grilled on hibachis). Leston
Havens, the great historian of psychiatry, talking about the
connection between hypnosis and hysteria. Did I mention it was
Halloween weekend? Was
that David Rosenhan or Phil Zimbardo dressed in a magician's
cape, cane, and top hat?
I don't remember those details anymore. But what I do
remember was that as soon as the festivities began, the Museum
staff told Martin that the cash bar was strictly illegal: this
was Pennsylvania, and there was no selling alcohol without a
state license. So
the bar had to be closed -- except that Bernard Raginsky
pulled out his checkbook and covered the whole expense. A great metaphor for
the commitment of individual members to the good of the
Society as a whole.
In my time with you today I want to return to my first point,
the relation between science and practice, and discuss a new
frontier for research in which scientists and practitioners
can collaborate, using hypnosis to expand our understanding of
the relations between mind and body.
 Across the history
of psychology and psychiatry, researchers of many different
theoretical stripes have found hypnosis intrinsically
interesting. And
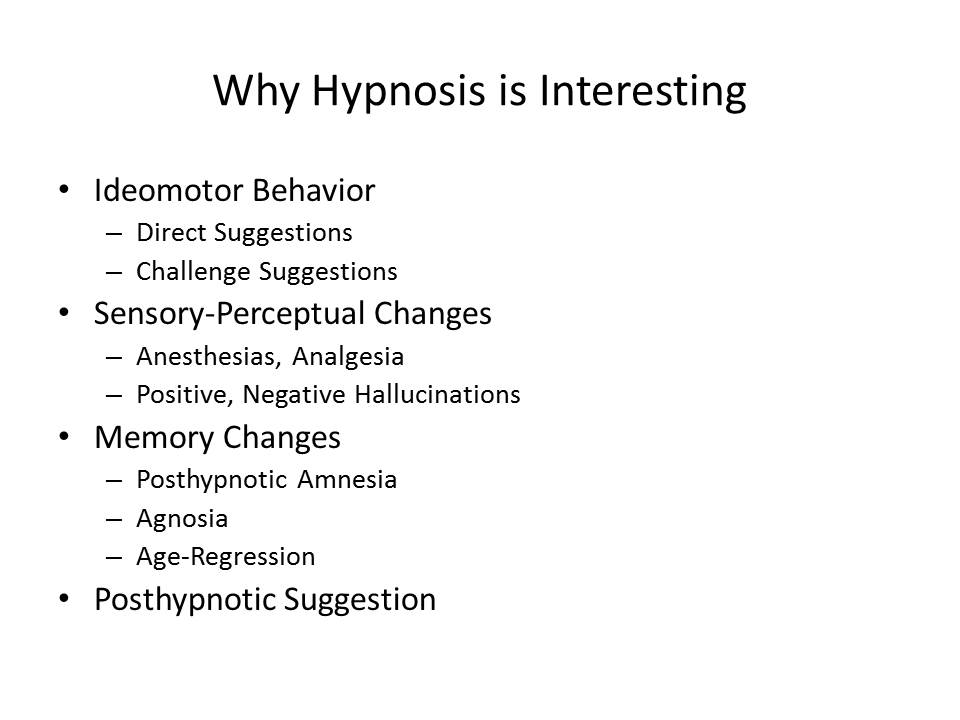
who wouldn't be interested in hypnosis? Hypnotic subjects
appear to lose control over voluntary motor activities; they
don't feel pain or touch, they go deaf or blind; they hear
voices that aren't there speaking to them, and they fail to
see things that are right there in front of them; they feel
like they're children again; they don't recognize objects that
should be familiar to them; they come out of hypnosis unable
to remember what they did while they were hypnotized; and when
the experimenter gives a pre-arranged cue, they carry out some
activity that had been suggested to them earlier, without
knowing what they're doing or why. Hypnosis is one of
the few things you can do in a laboratory that both
experimenter and subject find enjoyable -- at least if the
subject is highly hypnotizable; and even if he's not, it's
still a pleasant way to pass the time.
Across the history
of psychology and psychiatry, researchers of many different
theoretical stripes have found hypnosis intrinsically
interesting. And
who wouldn't be interested in hypnosis? Hypnotic subjects
appear to lose control over voluntary motor activities; they
don't feel pain or touch, they go deaf or blind; they hear
voices that aren't there speaking to them, and they fail to
see things that are right there in front of them; they feel
like they're children again; they don't recognize objects that
should be familiar to them; they come out of hypnosis unable
to remember what they did while they were hypnotized; and when
the experimenter gives a pre-arranged cue, they carry out some
activity that had been suggested to them earlier, without
knowing what they're doing or why. Hypnosis is one of
the few things you can do in a laboratory that both
experimenter and subject find enjoyable -- at least if the
subject is highly hypnotizable; and even if he's not, it's
still a pleasant way to pass the time.
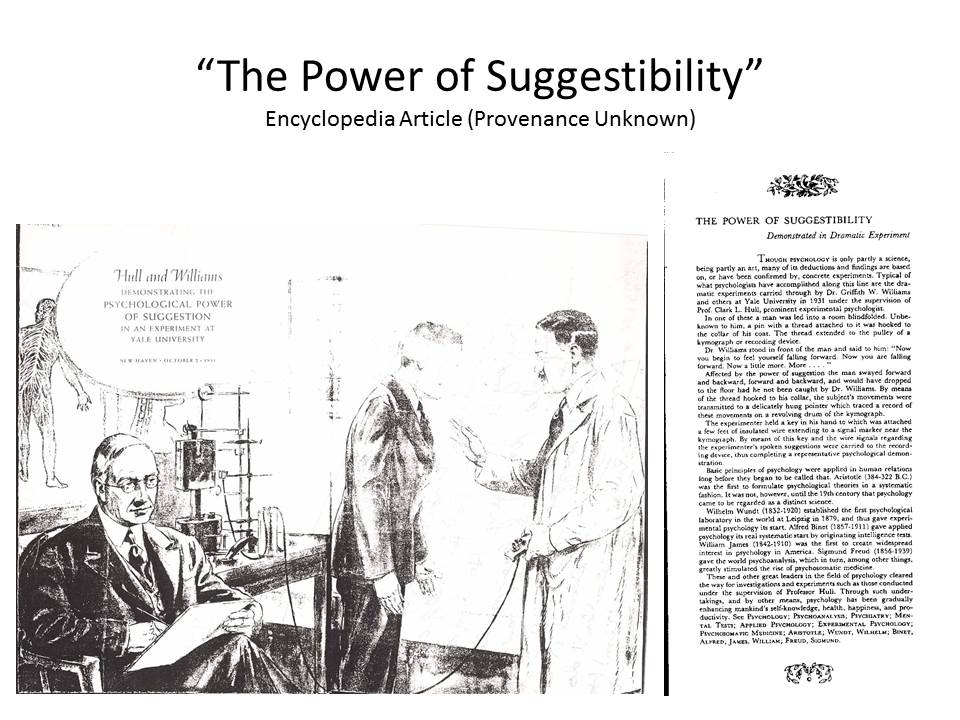 Sometimes, as in
the pioneering research of P.C. Young, hypnosis was just a
phenomenon to be studied with the laboratory methods of the
then-new science of psychology -- the goal being to find out
just what hypnosis can do and what it cannot (Young, 1925, 1926a, 1926b, 1927,
1931). This
was also the view of Clark L. Hull, who simply assumed that
hypnosis was a "habit phenomenon", something that the subject
got better at with practice, and who deployed his
sophisticated experimental methods to study hypnosis for its
own sake (Hull, 1933)
-- a project he abandoned in mid-course, leaving a legacy of
not 100, not 101, but 102 studies of hypnosis (Hull, 1930a, 1930b), and
another 40
studies on nonhypnotic suggestibility (Hull, 1929), most of which
remain undone to this day (and still worth doing, hint, hint)
. In much the
same way, I think it's fair to say that the "Golden Age" of
modern hypnosis research, beginning in the 1950s and running
into the 90s, was primarily concerned with applying
established paradigms and theories to the understanding of
hypnotic phenomena. Jack
Hilgard and Martin Orne, Ted Sarbin and Ted Barber, and their
progeny -- they had theories, for sure, but mostly they had
methods to match their curiosity about an intrinsically
interesting phenomenon.
Sometimes, as in
the pioneering research of P.C. Young, hypnosis was just a
phenomenon to be studied with the laboratory methods of the
then-new science of psychology -- the goal being to find out
just what hypnosis can do and what it cannot (Young, 1925, 1926a, 1926b, 1927,
1931). This
was also the view of Clark L. Hull, who simply assumed that
hypnosis was a "habit phenomenon", something that the subject
got better at with practice, and who deployed his
sophisticated experimental methods to study hypnosis for its
own sake (Hull, 1933)
-- a project he abandoned in mid-course, leaving a legacy of
not 100, not 101, but 102 studies of hypnosis (Hull, 1930a, 1930b), and
another 40
studies on nonhypnotic suggestibility (Hull, 1929), most of which
remain undone to this day (and still worth doing, hint, hint)
. In much the
same way, I think it's fair to say that the "Golden Age" of
modern hypnosis research, beginning in the 1950s and running
into the 90s, was primarily concerned with applying
established paradigms and theories to the understanding of
hypnotic phenomena. Jack
Hilgard and Martin Orne, Ted Sarbin and Ted Barber, and their
progeny -- they had theories, for sure, but mostly they had
methods to match their curiosity about an intrinsically
interesting phenomenon.
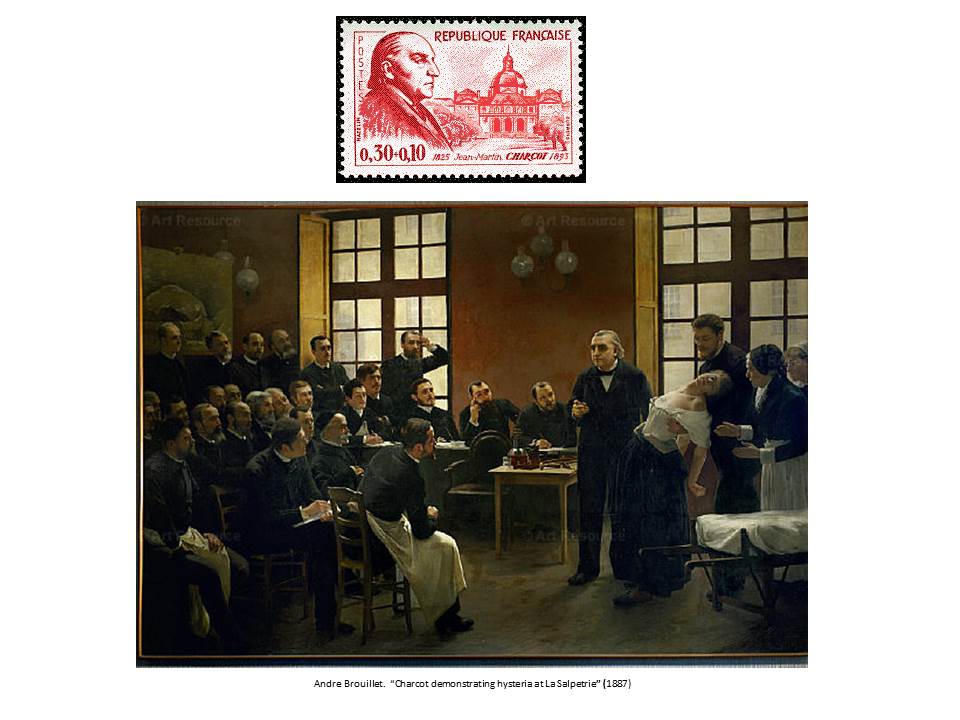 But this project, of
understanding hypnosis in terms of what is already known, has
coexisted with another project, which is to study hypnosis for
the unique light it can shed on mind and behavior. This has an even
longer history, extending to the clinical work of Charcot and
Janet, where hypnosis served as a kind of laboratory model for
understanding the mysteries of hysteria (Kihlstrom, 1979).
But this project, of
understanding hypnosis in terms of what is already known, has
coexisted with another project, which is to study hypnosis for
the unique light it can shed on mind and behavior. This has an even
longer history, extending to the clinical work of Charcot and
Janet, where hypnosis served as a kind of laboratory model for
understanding the mysteries of hysteria (Kihlstrom, 1979).
 William James devoted an
entire chapter of his Principles
(James, 1890/1980) to
hypnosis precisely because he thought the new scientific
psychology could benefit from the insights it provided (Kihlstrom & McConkey, 1990). James's interest in
hypnosis had its origins in his interest in the will, and he
thought that hypnosis could shed unique light on a basic
problem in psychology: how ideas, in the form of suggestions,
generated action, in the form of hypnotic behaviors. And, of course,
James was interested in consciousness. He thought that
consciousness and thinking were identical, and that
unconscious thought was a kind of oxymoron; still, he was
persuaded by Janet's observations, and his own, that in
hypnosis things could be unconsciously felt but not
consciously perceived, and that mental activity could be
divided into multiple streams, only one of which was
accessible to phenomenal awareness at any given time.
William James devoted an
entire chapter of his Principles
(James, 1890/1980) to
hypnosis precisely because he thought the new scientific
psychology could benefit from the insights it provided (Kihlstrom & McConkey, 1990). James's interest in
hypnosis had its origins in his interest in the will, and he
thought that hypnosis could shed unique light on a basic
problem in psychology: how ideas, in the form of suggestions,
generated action, in the form of hypnotic behaviors. And, of course,
James was interested in consciousness. He thought that
consciousness and thinking were identical, and that
unconscious thought was a kind of oxymoron; still, he was
persuaded by Janet's observations, and his own, that in
hypnosis things could be unconsciously felt but not
consciously perceived, and that mental activity could be
divided into multiple streams, only one of which was
accessible to phenomenal awareness at any given time.
 Both views -- the
relevance of hypnosis to motivation, and to consciousness --
were carried into the work of Jack Hilgard. At first, Hilgard's
interest in hypnosis was
carried over from his early work on learning, and especially
the distinction between voluntary and involuntary responses (Hilgard, 1948; Hilgard &
Marquis, 1940).
Like James, he thought that hypnosis was relevant to
motivation, and especially the translation of ideas into
action. His own
program of research had its origins in his interest in
psychodynamic theory, and the idea that behavior could arise
from unconscious ideas and motives (Hilgard, 1952, 1961). Finally, the
relevance to consciousness was expressed most clearly in his
"neodissociation" theory of divided consciousness (Hilgard, 1977).
Both views -- the
relevance of hypnosis to motivation, and to consciousness --
were carried into the work of Jack Hilgard. At first, Hilgard's
interest in hypnosis was
carried over from his early work on learning, and especially
the distinction between voluntary and involuntary responses (Hilgard, 1948; Hilgard &
Marquis, 1940).
Like James, he thought that hypnosis was relevant to
motivation, and especially the translation of ideas into
action. His own
program of research had its origins in his interest in
psychodynamic theory, and the idea that behavior could arise
from unconscious ideas and motives (Hilgard, 1952, 1961). Finally, the
relevance to consciousness was expressed most clearly in his
"neodissociation" theory of divided consciousness (Hilgard, 1977).
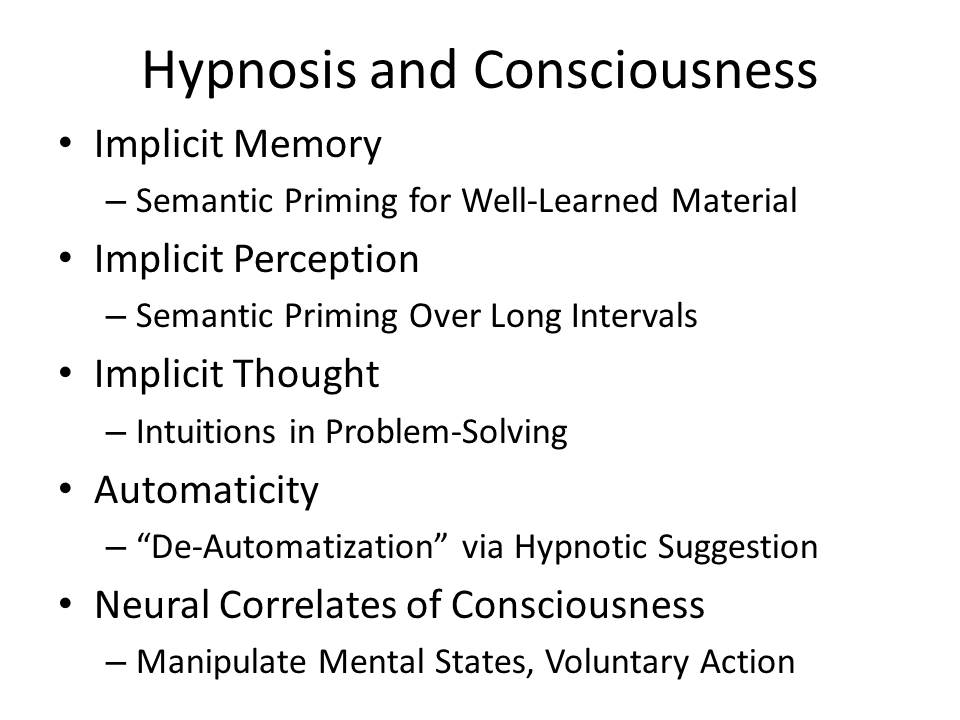 Over the years,
hypnosis has offered much to psychological theory, and
particularly to our understanding of consciousness (Kihlstrom, 2007, 2013). Studies of
posthypnotic amnesia, hypnotic blindness, for example, offer a
new perspective on unconscious memory and perception. Most studies of
implicit memory require relatively impoverished encoding
conditions, and are limited to what is known as repetition
priming -- which, frankly, is not a very interesting form of
memory. But with
hypnosis we can get semantic priming even for well-learned
material. This
shows us that unconscious memory can occur even with richly
elaborated, organized material.
Similarly, most studies of implicit perception degrade
the stimulus through such techniques as masking, which
effectively preclude the subject from analyzing the stimulus
effectively, so that when you get semantic priming, it's
analytically limited and doesn't last very long. Not so in hypnotic
blindness and deafness -- which, again, indicates that
unconscious perception can occur even when the subject can
devote full attentional resources to processing the stimulus. Kenneth Bowers'
seminal studies of intuition, which shed new on the nature and
scope of unconscious thinking, were directly inspired by his
earlier studies of posthypnotic suggestion. And then, finally,
we have recent studies of the effects of hypnotic agnosia on
performance on the Stroop task -- which indicate that mental
processes, once automatized and rendered unconscious, can be de-automatized
and performed consciously.
Over the years,
hypnosis has offered much to psychological theory, and
particularly to our understanding of consciousness (Kihlstrom, 2007, 2013). Studies of
posthypnotic amnesia, hypnotic blindness, for example, offer a
new perspective on unconscious memory and perception. Most studies of
implicit memory require relatively impoverished encoding
conditions, and are limited to what is known as repetition
priming -- which, frankly, is not a very interesting form of
memory. But with
hypnosis we can get semantic priming even for well-learned
material. This
shows us that unconscious memory can occur even with richly
elaborated, organized material.
Similarly, most studies of implicit perception degrade
the stimulus through such techniques as masking, which
effectively preclude the subject from analyzing the stimulus
effectively, so that when you get semantic priming, it's
analytically limited and doesn't last very long. Not so in hypnotic
blindness and deafness -- which, again, indicates that
unconscious perception can occur even when the subject can
devote full attentional resources to processing the stimulus. Kenneth Bowers'
seminal studies of intuition, which shed new on the nature and
scope of unconscious thinking, were directly inspired by his
earlier studies of posthypnotic suggestion. And then, finally,
we have recent studies of the effects of hypnotic agnosia on
performance on the Stroop task -- which indicate that mental
processes, once automatized and rendered unconscious, can be de-automatized
and performed consciously.
And that's not all. Hypnosis
has also made important contributions to theory in personality
and social psychology, developmental psychology, and, of
course, clinical psychology.
 I won't detail these further, because I
want to dwell for a considerable amount of time on what I
think is a new frontier for hypnosis research, which allies
both scientists and practitioners: psychosomatic medicine, a
field predicated on the idea that patients' feelings and
beliefs can affect the functioning of their bodies (Harrington, 2008). This reveals another
side of the mind-body problem.
Ever since Descartes, science has been consumed by the
question of how, or even whether, mental
states are produced by bodily processes -- a problem which is
now generally known as the neural correlates of consciousness. But in
psychosomatics, we're interested in the reverse: whether, and
if so how, mental states affect bodily processes.
I won't detail these further, because I
want to dwell for a considerable amount of time on what I
think is a new frontier for hypnosis research, which allies
both scientists and practitioners: psychosomatic medicine, a
field predicated on the idea that patients' feelings and
beliefs can affect the functioning of their bodies (Harrington, 2008). This reveals another
side of the mind-body problem.
Ever since Descartes, science has been consumed by the
question of how, or even whether, mental
states are produced by bodily processes -- a problem which is
now generally known as the neural correlates of consciousness. But in
psychosomatics, we're interested in the reverse: whether, and
if so how, mental states affect bodily processes.
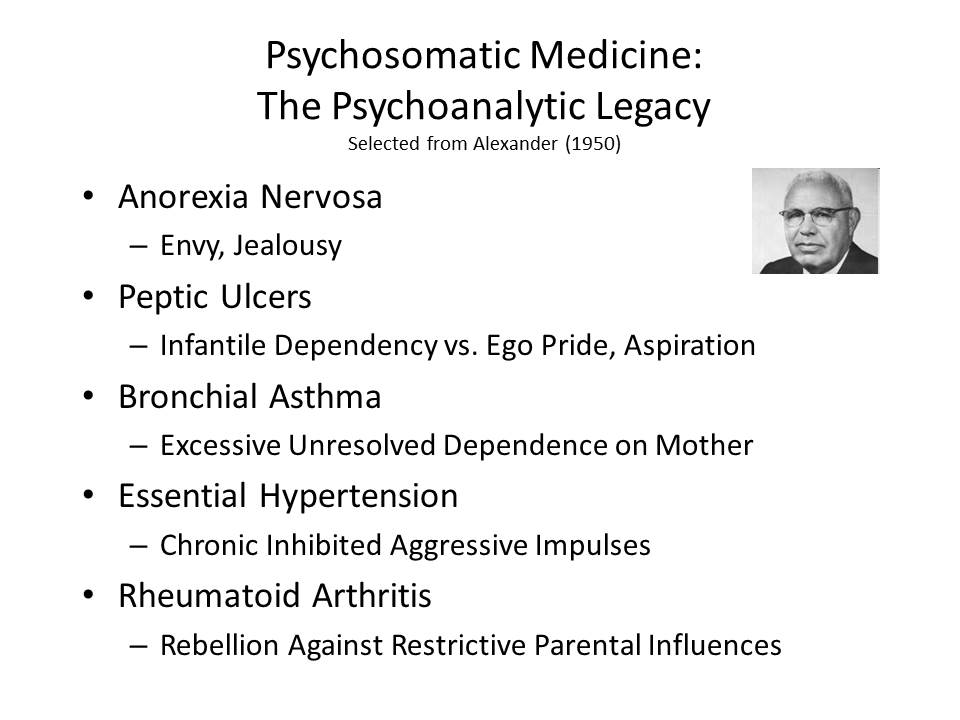 Now, psychosomatic medicine is
in bad odor in psychiatry and clinical psychology these days
-- in part, to be honest, because of the excesses of
psychoanalytic theory, which held, among other things, that
bronchial asthma was caused by excessive unresolved dependence
on one's mother (Alexander,
1950).
Now, psychosomatic medicine is
in bad odor in psychiatry and clinical psychology these days
-- in part, to be honest, because of the excesses of
psychoanalytic theory, which held, among other things, that
bronchial asthma was caused by excessive unresolved dependence
on one's mother (Alexander,
1950).
 But much of the blame also
falls on the biological revolution in psychiatry, and the
general reluctance of most physicians, even psychiatrists, to
take psychosocial processes seriously. Consider, for
example, the proclivity of so many mental-health professionals
to dispense medication to their depressed and anxious
patients, and the reluctance of insurance companies to pay for
much by way of psychotherapy -- even under health care reform.
I have remarked
elsewhere that the ideal to which many physicians seem to
aspire is the "feinberger" (or medical "tricorder") and
surgical bio-bed used by Dr. McCoy in the Star Trek series,
which permitted the diagnosis and treatment of illness without
speaking to or touching the patient (Kihlstrom, 2003, 2008). Too many physicians
appear to be threatened by the notion that the physical state of
their patients could be affected by the mental state of their
patients, and they'd like to get rid of psychosomatics by
whatever means necessary.
Present company excepted, of course: hypnosis teaches
us to talk, and listen, to our patients.
But much of the blame also
falls on the biological revolution in psychiatry, and the
general reluctance of most physicians, even psychiatrists, to
take psychosocial processes seriously. Consider, for
example, the proclivity of so many mental-health professionals
to dispense medication to their depressed and anxious
patients, and the reluctance of insurance companies to pay for
much by way of psychotherapy -- even under health care reform.
I have remarked
elsewhere that the ideal to which many physicians seem to
aspire is the "feinberger" (or medical "tricorder") and
surgical bio-bed used by Dr. McCoy in the Star Trek series,
which permitted the diagnosis and treatment of illness without
speaking to or touching the patient (Kihlstrom, 2003, 2008). Too many physicians
appear to be threatened by the notion that the physical state of
their patients could be affected by the mental state of their
patients, and they'd like to get rid of psychosomatics by
whatever means necessary.
Present company excepted, of course: hypnosis teaches
us to talk, and listen, to our patients.
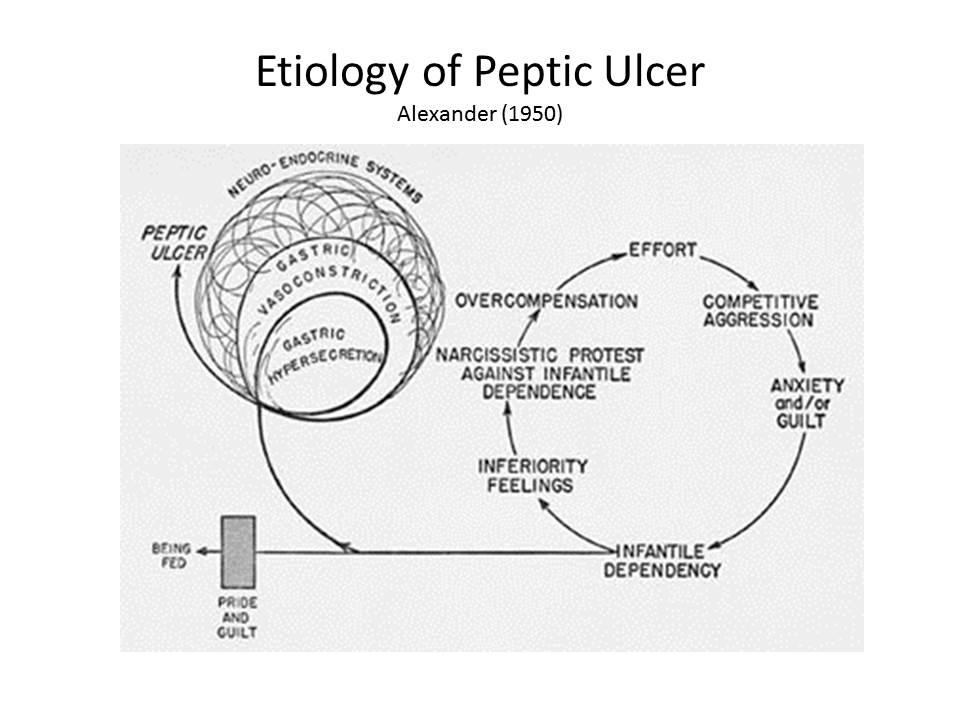 As
a case in point, consider the status of stomach ulcers. The traditional
psychoanalytic formulation is that peptic ulcers arise from an
unconscious conflict between infantile dependency and ego
pride (Alexander, 1950).
As
a case in point, consider the status of stomach ulcers. The traditional
psychoanalytic formulation is that peptic ulcers arise from an
unconscious conflict between infantile dependency and ego
pride (Alexander, 1950).
It's easy to make fun of such proposals now, but -- as Susan
Sontag reminded us in Illness as Metaphor (1978), it
was not that long ago that psychiatrists proposed that
cancer was itself psychosomatic, caused by people who
bottled their emotions up so tightly that they burst forth
as tumors.
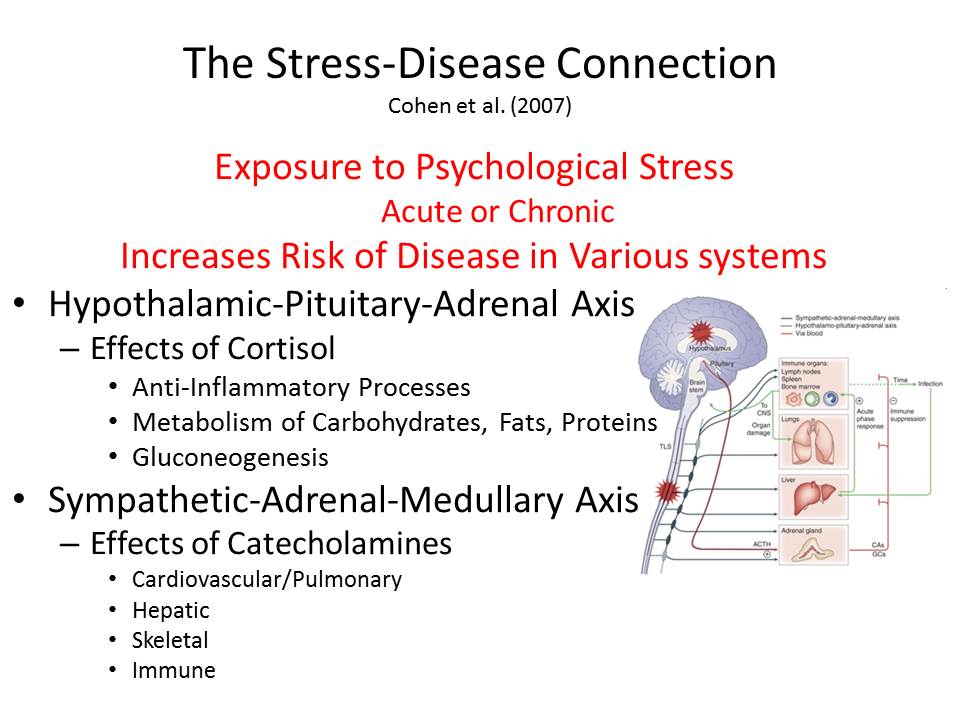 A more recent view implicates
stress of any kind, mediated through the "flight or fight"
reaction. As
such, it exemplifies what we can call the stress-disease
connection (Cohen, Janicki-Deverts, &
Miller, 2007) mediated by the
hypothalamic-pituitary-adrenocortical axis (HPA) or the
sympathetic-adrenal-medullary axis (SAM).
A more recent view implicates
stress of any kind, mediated through the "flight or fight"
reaction. As
such, it exemplifies what we can call the stress-disease
connection (Cohen, Janicki-Deverts, &
Miller, 2007) mediated by the
hypothalamic-pituitary-adrenocortical axis (HPA) or the
sympathetic-adrenal-medullary axis (SAM).
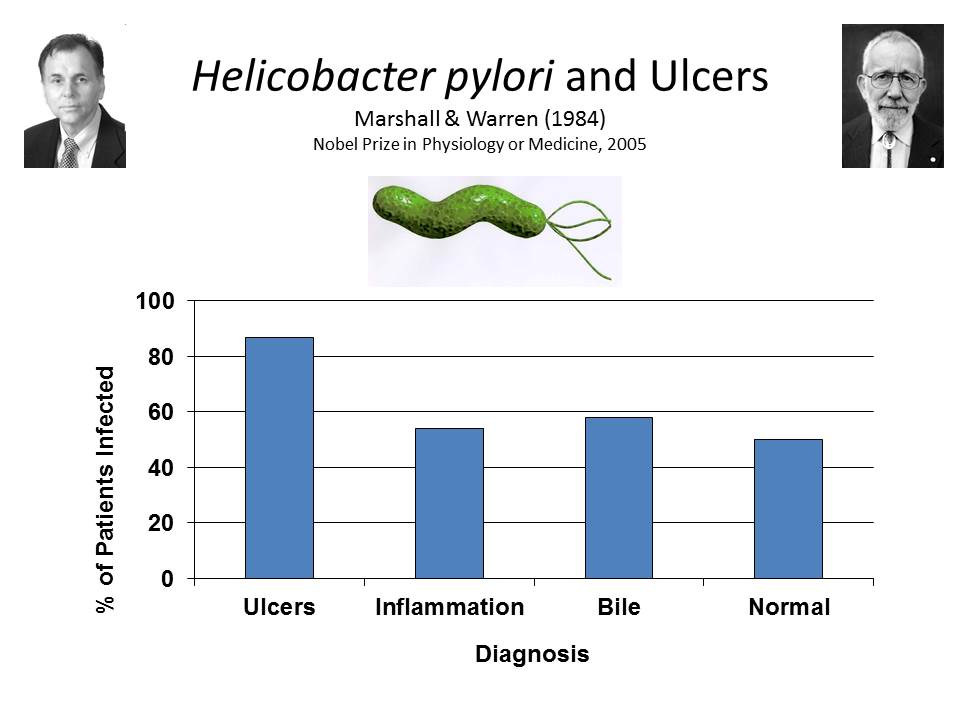 Both views were
challenged by discovery, in the 1980s, of an association
between peptic ulcers and infection with a bacterium known as
helicobacter pylori
-- work that won the 2005 Nobel Prize in Physiology or
Medicine for Barry Marshall and Robin Warren (Marshall & Warren, 1984).
Both views were
challenged by discovery, in the 1980s, of an association
between peptic ulcers and infection with a bacterium known as
helicobacter pylori
-- work that won the 2005 Nobel Prize in Physiology or
Medicine for Barry Marshall and Robin Warren (Marshall & Warren, 1984).
 After Marshall and
Warren published their discovery, Steven Hyman, a leading
molecular neuropsychiatrist, soon to become the Director of
the National Institute of Mental Health, later Provost of
Harvard University, and currently the Director of the Stanley Center for Psychiatric Research at
Harvard and MIT, wrote a commentary entitled "Another One
Bites the Dust" celebrating the triumph of biomedicine over
psychology (Hyman, 1994).
After Marshall and
Warren published their discovery, Steven Hyman, a leading
molecular neuropsychiatrist, soon to become the Director of
the National Institute of Mental Health, later Provost of
Harvard University, and currently the Director of the Stanley Center for Psychiatric Research at
Harvard and MIT, wrote a commentary entitled "Another One
Bites the Dust" celebrating the triumph of biomedicine over
psychology (Hyman, 1994).
 Hyman's paper
epitomizes the biological and pharmacological revolution in
mental health. The
same attitude is reflected in a famous aphorism attributed
to Ralph Gerard, founder of the Society for Neuroscience,
that "behind every twisted thought there lies a twisted
molecule" (Healy, 2004).
And, more recently, in the promise of Thomas Insel,
the current Director of the National Institute of Mental
Health, that the key to mental illness will be found in the
Human Connectome, rather than in any analysis of human
experience, thought, and action (Insel, 2010).
Hyman's paper
epitomizes the biological and pharmacological revolution in
mental health. The
same attitude is reflected in a famous aphorism attributed
to Ralph Gerard, founder of the Society for Neuroscience,
that "behind every twisted thought there lies a twisted
molecule" (Healy, 2004).
And, more recently, in the promise of Thomas Insel,
the current Director of the National Institute of Mental
Health, that the key to mental illness will be found in the
Human Connectome, rather than in any analysis of human
experience, thought, and action (Insel, 2010).
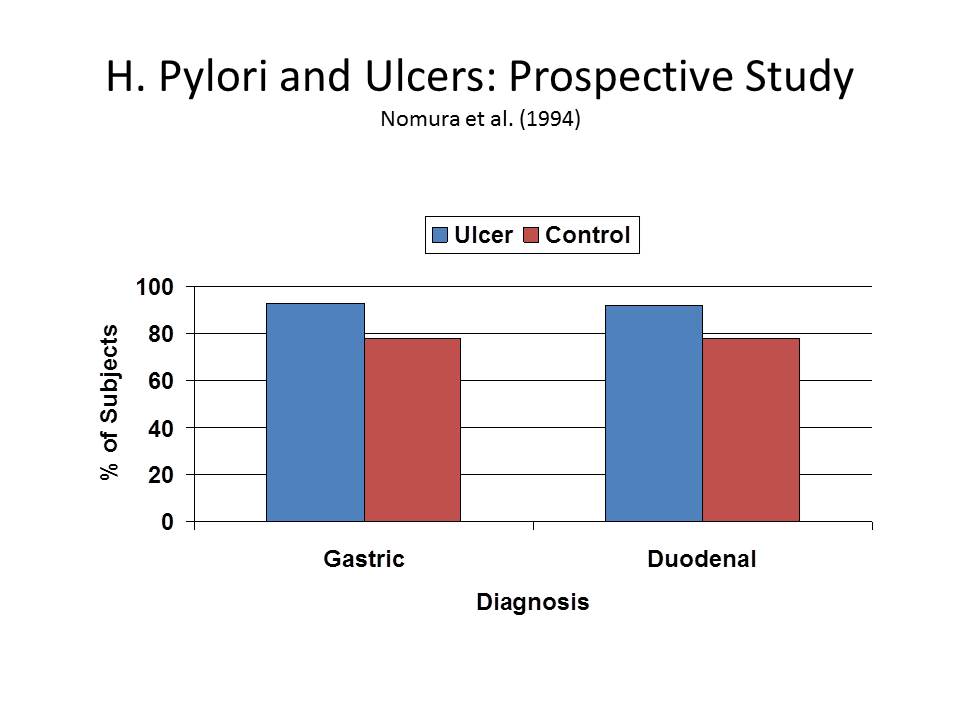 But not so fast. It turns out that,
while antibodies for H.
pylori infection are found in over 90% of ulcer
patients, they are also found in almost 80% of ulcer-free
patients, leading one group of researchers to conclude that
"other factors in addition to H. pylori
infection have an important role in the development of
peptic ulcer" (Nomura,
Stemmermann, Chyou, Perez-Perez, & Blaser, 1994).
But not so fast. It turns out that,
while antibodies for H.
pylori infection are found in over 90% of ulcer
patients, they are also found in almost 80% of ulcer-free
patients, leading one group of researchers to conclude that
"other factors in addition to H. pylori
infection have an important role in the development of
peptic ulcer" (Nomura,
Stemmermann, Chyou, Perez-Perez, & Blaser, 1994).
 Moreover,
Bruce Overmier and Robert Murison have developed an animal
model of ulcers which clearly shows that stress, in the form
of unpredictable and uncontrollable foot shock, clearly
"precipitates and sustains" gastric ulceration (Overmier & Murison, 2013). In their model, h. pylori may
increase vulnerability to gastric secretions, but it is not
their sole cause. The
effects of stress on the body may be mediated by the HPA and
SAM, in physiological terms, but stress is fundamentally a
mental state, involving the organism's perception of
environmental challenges.
Moreover,
Bruce Overmier and Robert Murison have developed an animal
model of ulcers which clearly shows that stress, in the form
of unpredictable and uncontrollable foot shock, clearly
"precipitates and sustains" gastric ulceration (Overmier & Murison, 2013). In their model, h. pylori may
increase vulnerability to gastric secretions, but it is not
their sole cause. The
effects of stress on the body may be mediated by the HPA and
SAM, in physiological terms, but stress is fundamentally a
mental state, involving the organism's perception of
environmental challenges.
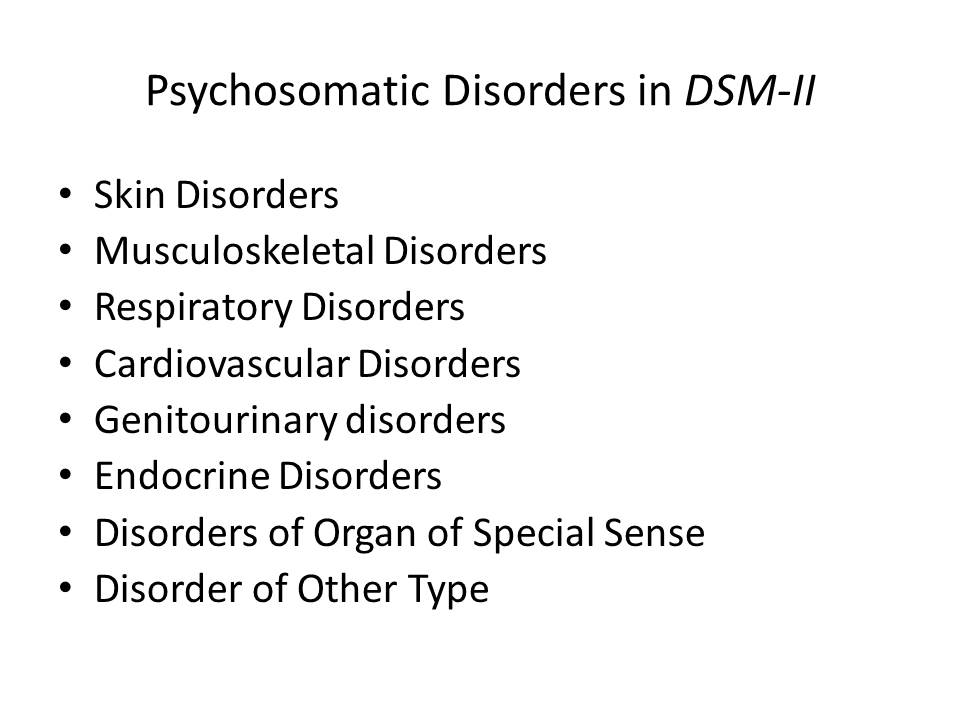 The evolution
of the Diagnostic and
Statistical Manual of Mental Disorders (DSM) also illustrates
the problem. The
first two editions of DSM,
published in 1952 and 1968, respectively, listed the
psychosomatic disorders in their own special section --
perhaps owing to the influence of psychoanalysis.
The evolution
of the Diagnostic and
Statistical Manual of Mental Disorders (DSM) also illustrates
the problem. The
first two editions of DSM,
published in 1952 and 1968, respectively, listed the
psychosomatic disorders in their own special section --
perhaps owing to the influence of psychoanalysis.
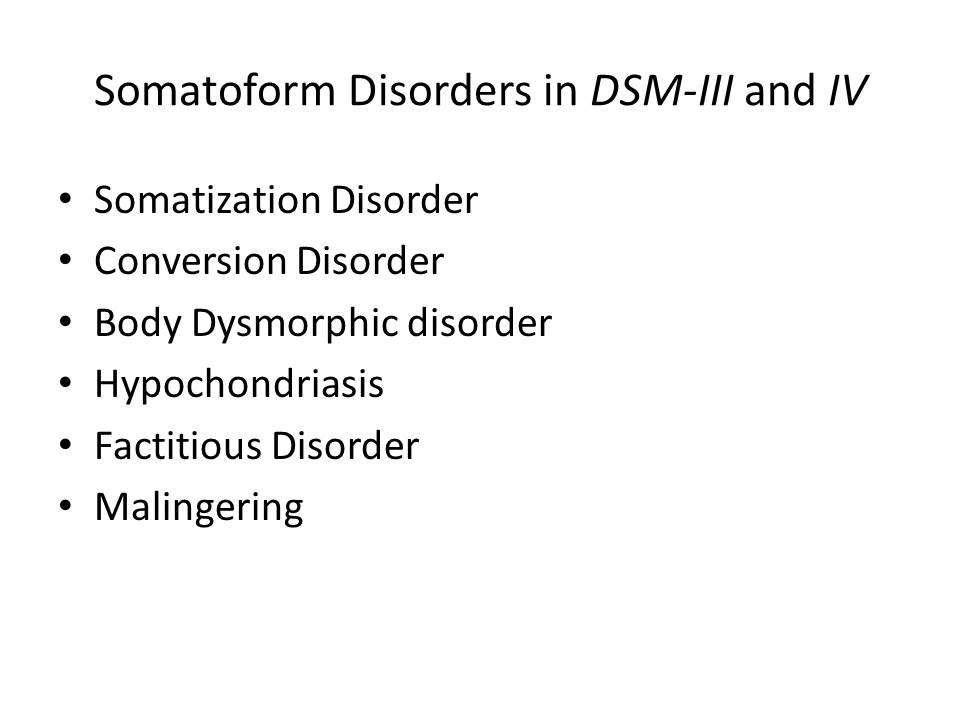 But the
entire category was dropped in DSM-III, essentially
relegating the psychosomatic disorders to a footnote. In this respect, at
least, the later editions of DSM made a big
mistake, creating a diagnostic category that -- to adopt the
language of Kurt Vonnegut (in Cat's Cradle, 1963)
-- is more a granfaloon
than a karass In the first
place, the conversion disorders reflect pseudoneurological
problems with specific aspects of consciousness, either
conscious awareness of sensations and percepts or conscious
control of motor function, and properly belong with the
dissociative disorders (Kihlstrom,
1994). The
somatoform disorders, including somatization disorder and
hypochondriasis, are instances where the patient has multiple
unexplained physical complaints that really serve to
communicate emotional distress, or to manipulate other people
(Kihlstrom & Canter
Kihlstrom, 1999).
The complaints are medically unexplained, meaning that
physical examination and diagnostic testing reveals that
there's nothing wrong with the body. But in the
psychosomatic disorders there is definitely
something wrong with some specific bodily function: in ulcers,
for example, there are those nasty lesions in the lining of
the small intestine and the stomach. They're not just
somatoform --
they're somatic for
real. And
they don't just "contribute" to the patient's medical
condition: They cause
it to begin with.
But the
entire category was dropped in DSM-III, essentially
relegating the psychosomatic disorders to a footnote. In this respect, at
least, the later editions of DSM made a big
mistake, creating a diagnostic category that -- to adopt the
language of Kurt Vonnegut (in Cat's Cradle, 1963)
-- is more a granfaloon
than a karass In the first
place, the conversion disorders reflect pseudoneurological
problems with specific aspects of consciousness, either
conscious awareness of sensations and percepts or conscious
control of motor function, and properly belong with the
dissociative disorders (Kihlstrom,
1994). The
somatoform disorders, including somatization disorder and
hypochondriasis, are instances where the patient has multiple
unexplained physical complaints that really serve to
communicate emotional distress, or to manipulate other people
(Kihlstrom & Canter
Kihlstrom, 1999).
The complaints are medically unexplained, meaning that
physical examination and diagnostic testing reveals that
there's nothing wrong with the body. But in the
psychosomatic disorders there is definitely
something wrong with some specific bodily function: in ulcers,
for example, there are those nasty lesions in the lining of
the small intestine and the stomach. They're not just
somatoform --
they're somatic for
real. And
they don't just "contribute" to the patient's medical
condition: They cause
it to begin with.
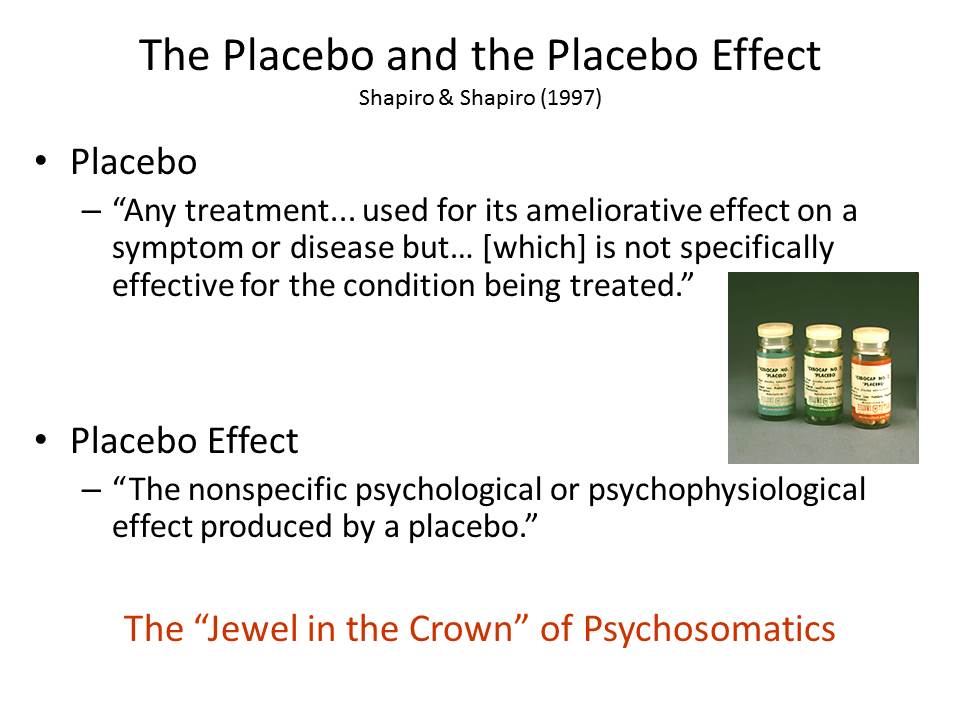 And
finally, there is the placebo effect -- sometimes called the
"crown jewel" of psychosomatic medicine, because it reveals
the effects of mental states -- attitudes, beliefs, and
expectations, feelings and motives -- on physical outcomes (Beecher, 1955; Harrington, 1997;
Shapiro & Shapiro, 1997). Note, first, that
the clinical trials that validate new drugs, devices, or
procedures virtually mandate a comparison to placebo. The implication is
that placebo effects are something to be done away with,
rather than capitalized on.
And
finally, there is the placebo effect -- sometimes called the
"crown jewel" of psychosomatic medicine, because it reveals
the effects of mental states -- attitudes, beliefs, and
expectations, feelings and motives -- on physical outcomes (Beecher, 1955; Harrington, 1997;
Shapiro & Shapiro, 1997). Note, first, that
the clinical trials that validate new drugs, devices, or
procedures virtually mandate a comparison to placebo. The implication is
that placebo effects are something to be done away with,
rather than capitalized on.
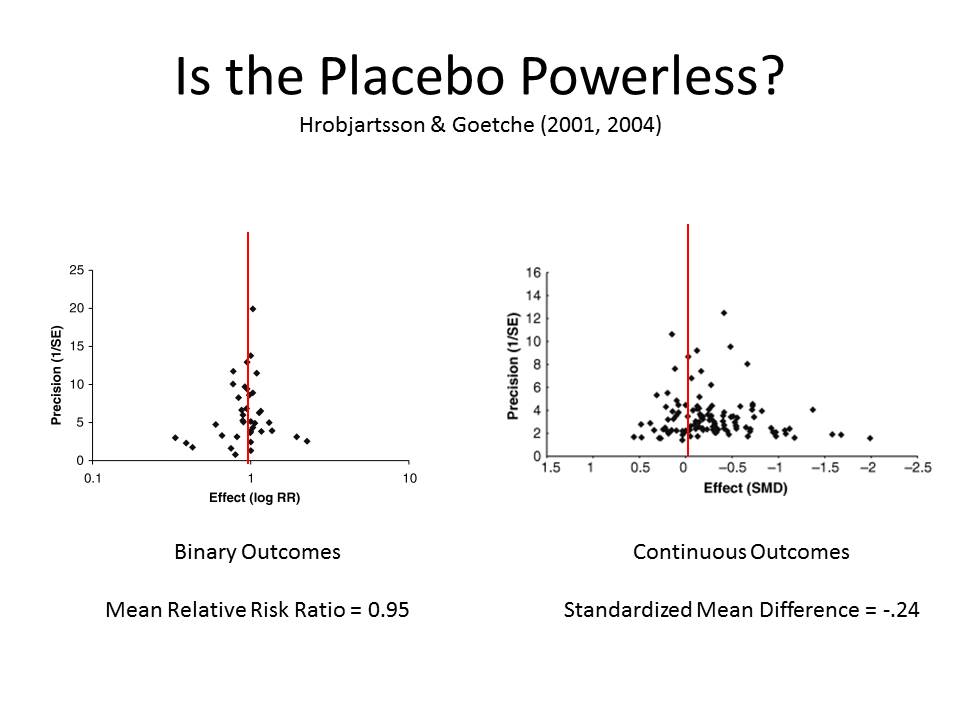 Placebo
effects themselves aren't of substantive interest, which is
why Hrobjartsson and Gotszche were able to find only 114
studies in the whole medical literature that compared placebo
to a no-treatment control
(Hrobjartsson & Gotzsche, 2001a, 2001b). And, of course, for
all the attention paid to placebo effects in both the popular
and professional press, these authors -- perhaps with relief,
perhaps with glee -- found scant evidence of a placebo effect
on any biological endpoint, such as nausea, asthma, or
hypertension. Placebos
may make people feel
better -- though, frankly, Hrobjartsson and Goetsche doubt
even that; but they don't seem to actually get better. This is a real
challenge for placebo research -- to show that placebos and
other psychological interventions can have an effect on
somatic functioning (Price,
Finniss, & Benedetti, 2008).
Placebo
effects themselves aren't of substantive interest, which is
why Hrobjartsson and Gotszche were able to find only 114
studies in the whole medical literature that compared placebo
to a no-treatment control
(Hrobjartsson & Gotzsche, 2001a, 2001b). And, of course, for
all the attention paid to placebo effects in both the popular
and professional press, these authors -- perhaps with relief,
perhaps with glee -- found scant evidence of a placebo effect
on any biological endpoint, such as nausea, asthma, or
hypertension. Placebos
may make people feel
better -- though, frankly, Hrobjartsson and Goetsche doubt
even that; but they don't seem to actually get better. This is a real
challenge for placebo research -- to show that placebos and
other psychological interventions can have an effect on
somatic functioning (Price,
Finniss, & Benedetti, 2008).
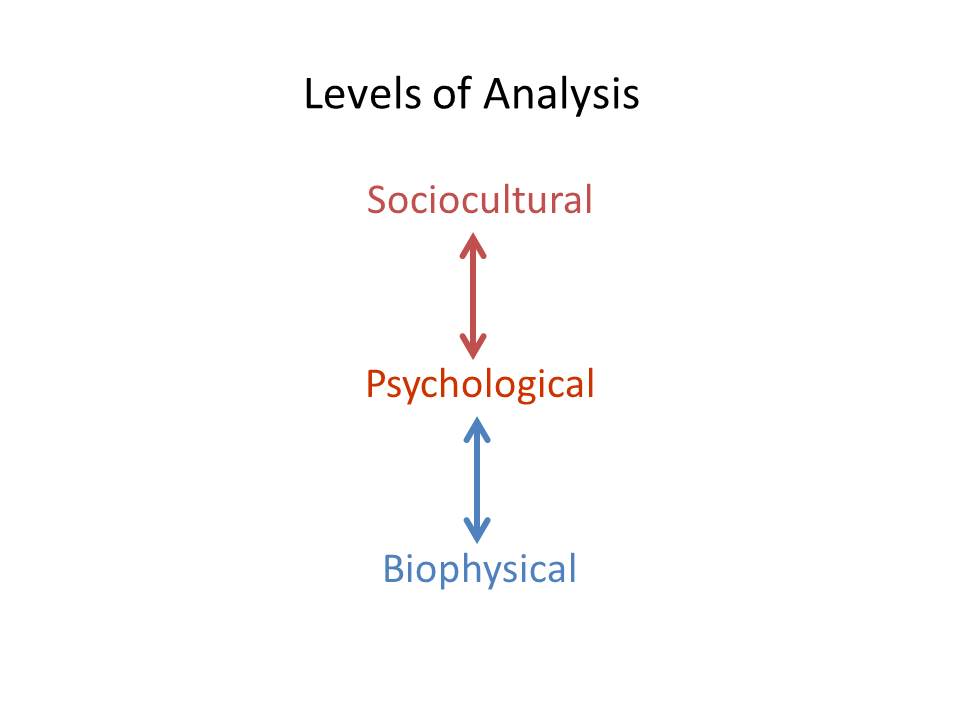 Let me be
clearer about what I mean -- and you'll have to pardon the
dualism in what I'm about to say. After all, I'm
a psychologist, and psychology is essentially dualistic in
nature: as William James (James,
1890/1980) (p. 1) understood. Psychology is the
science of mental life, and we can do our work at the
psychological level of analysis without ever asking how the
brain does it. That's
a different level of analysis, and while the neural basis of
mental life is interesting, psychologists are under no
obligation to study it. "Neodualists"
like myself acknowledge that the mind has its biological basis
in the brain, but insist that mental life can be analyzed at
its own level, without reduction to biology or physics. Or, as Ulric Neisser
famously put it, psychology isn't "just something to do until
the biochemist comes" (Neisser,
1967) (p. 1).
Let me be
clearer about what I mean -- and you'll have to pardon the
dualism in what I'm about to say. After all, I'm
a psychologist, and psychology is essentially dualistic in
nature: as William James (James,
1890/1980) (p. 1) understood. Psychology is the
science of mental life, and we can do our work at the
psychological level of analysis without ever asking how the
brain does it. That's
a different level of analysis, and while the neural basis of
mental life is interesting, psychologists are under no
obligation to study it. "Neodualists"
like myself acknowledge that the mind has its biological basis
in the brain, but insist that mental life can be analyzed at
its own level, without reduction to biology or physics. Or, as Ulric Neisser
famously put it, psychology isn't "just something to do until
the biochemist comes" (Neisser,
1967) (p. 1).
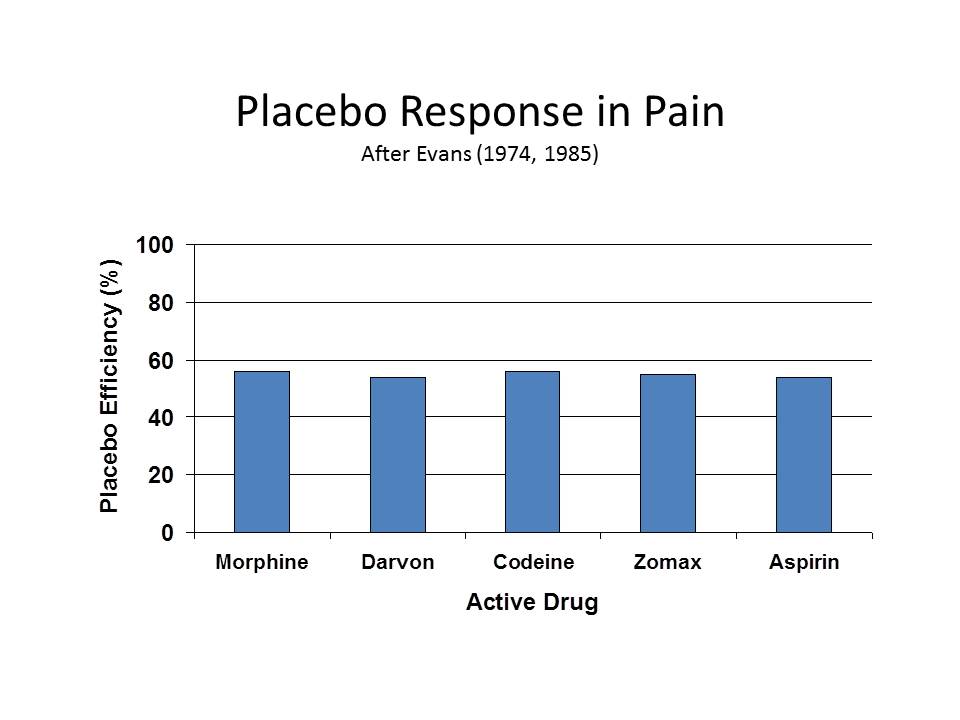 Anyway, placebo and other
psychosomatic effects have their origins in the person's
mental state -- his or her knowledge or beliefs, attitudes and
expectancies, feelings and drives. The best-documented
placebo effects, undoubted even by Hrobjartsson and Gotszche,
are in the domains of pain and depression. As Fred Evans (Evans, 1974) and others
have shown, big, dark-colored, bad-tasting, expensive placebos
are more effective than small, brightly colored, good-tasting,
discounted ones; placebos delivered intravenously are more
powerful than those delivered intramuscularly or orally; and,
beautifully, the magnitude of the placebo effect is a constant
proportion of the active agent to which it is being compared
(roughly 55%). And
as Irving Kirsch famously found, the bulk of the effect of
most antidepressant drugs currently on the market is accounted
for by placebo effects (Kirsch,
Moore, Scoboria, & Nicholls, 2002). The same is probably
true for anxiolytics. But
pain, depression, and anxiety are mental states, and they
don't count as psychosomatic effects. To count as
psychosomatic, we have to have evidence that suggestion and
belief influence actual bodily functioning.
Anyway, placebo and other
psychosomatic effects have their origins in the person's
mental state -- his or her knowledge or beliefs, attitudes and
expectancies, feelings and drives. The best-documented
placebo effects, undoubted even by Hrobjartsson and Gotszche,
are in the domains of pain and depression. As Fred Evans (Evans, 1974) and others
have shown, big, dark-colored, bad-tasting, expensive placebos
are more effective than small, brightly colored, good-tasting,
discounted ones; placebos delivered intravenously are more
powerful than those delivered intramuscularly or orally; and,
beautifully, the magnitude of the placebo effect is a constant
proportion of the active agent to which it is being compared
(roughly 55%). And
as Irving Kirsch famously found, the bulk of the effect of
most antidepressant drugs currently on the market is accounted
for by placebo effects (Kirsch,
Moore, Scoboria, & Nicholls, 2002). The same is probably
true for anxiolytics. But
pain, depression, and anxiety are mental states, and they
don't count as psychosomatic effects. To count as
psychosomatic, we have to have evidence that suggestion and
belief influence actual bodily functioning.
 But that's not all we have to
show, because every mental state is associated with some
neural state -- even diehard dualists acknowledge this, as in
Leibnitz's doctrine of psychophysical parallelism. In that sense, we're
all materialists now, even if we don't have a complete grasp
of how brain states cause mental states -- and even if we
prefer to confine our research and theories to the
psychological level of analysis.
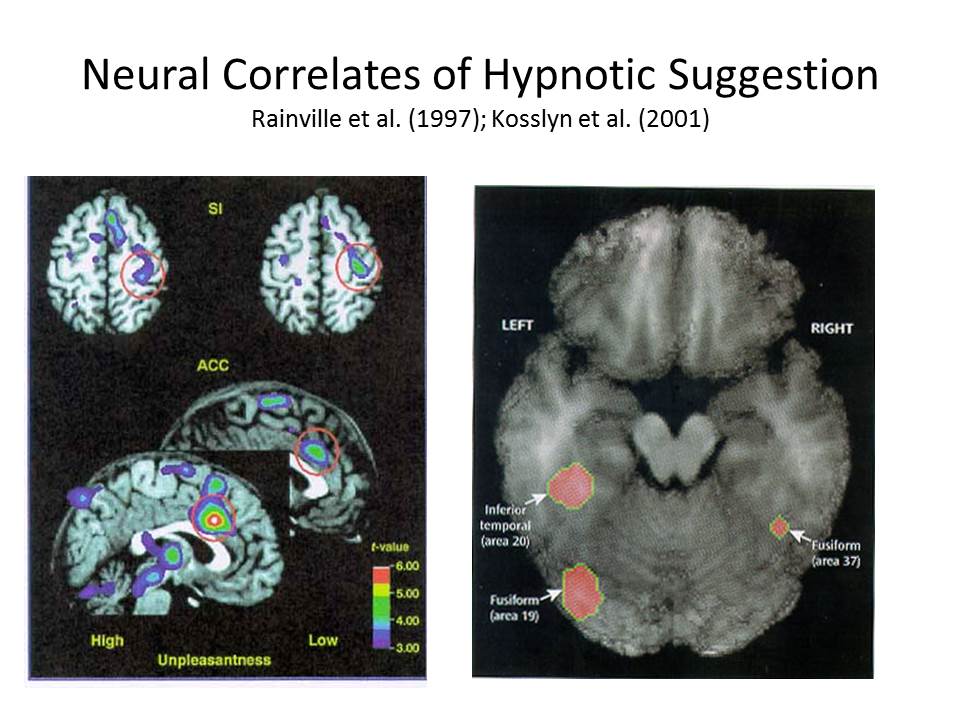
So, when a brain-imaging study finds that hypnotic
analgesia is associated with changes in the somatosensory
cortex or the anterior cingulate gyrus (Rainville, Hofbauer, Bushnell,
Duncan, & Price, 2002), or that hypnotic color
blindness is associated with changes in area V4 of
extra-striate cortex (Kosslyn,
Thompson, Costantini-Ferrando, Alpert, & Spiegel, 2000),
that should surprise nobody -- except those who think that
hypnotic subjects don't really experience subjectively
compelling changes in perception. Any change in mental
state must be
associated with a change in brain state, for the simple reason
that "the mind is what
the brain does" (Minsky,
1987).
But that's not all we have to
show, because every mental state is associated with some
neural state -- even diehard dualists acknowledge this, as in
Leibnitz's doctrine of psychophysical parallelism. In that sense, we're
all materialists now, even if we don't have a complete grasp
of how brain states cause mental states -- and even if we
prefer to confine our research and theories to the
psychological level of analysis.
So, when a brain-imaging study finds that hypnotic
analgesia is associated with changes in the somatosensory
cortex or the anterior cingulate gyrus (Rainville, Hofbauer, Bushnell,
Duncan, & Price, 2002), or that hypnotic color
blindness is associated with changes in area V4 of
extra-striate cortex (Kosslyn,
Thompson, Costantini-Ferrando, Alpert, & Spiegel, 2000),
that should surprise nobody -- except those who think that
hypnotic subjects don't really experience subjectively
compelling changes in perception. Any change in mental
state must be
associated with a change in brain state, for the simple reason
that "the mind is what
the brain does" (Minsky,
1987).
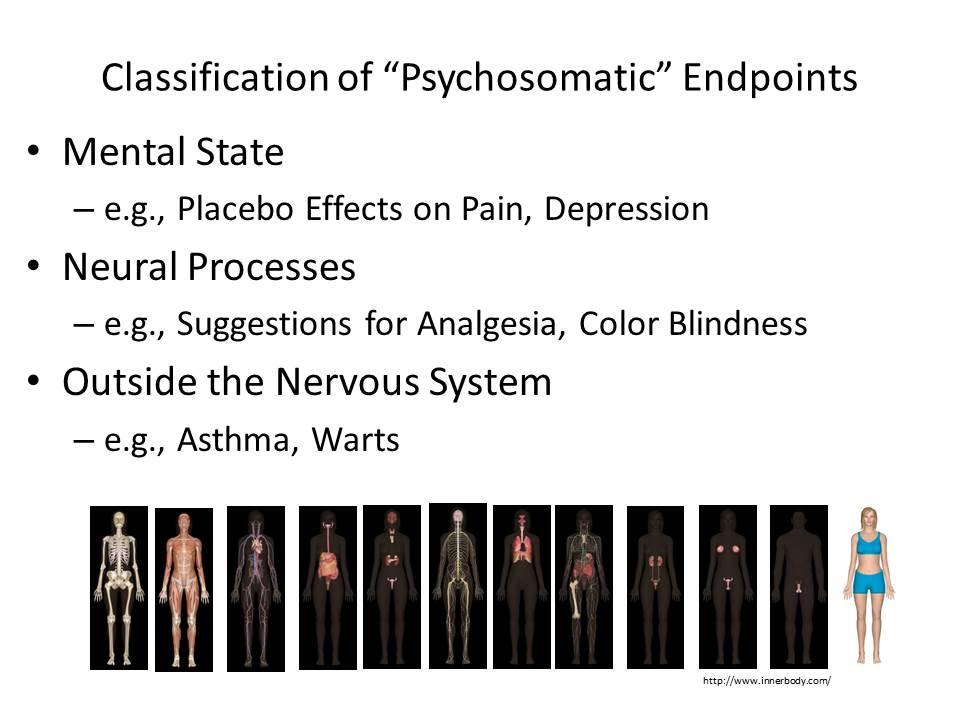 So if we
really want to demonstrate psychosomatic effects, we've got to
get out of the nervous system, and into other systems of the
body -- like the gastrointestinal system, in the case of
psychosomatic ulcers. And
here's where hypnosis comes in, because we have a long history
of obtaining such effects with hypnosis (Black, 1969; Bowers & Kelly,
1979; Covino, 2008; Covino & Pinnell, 2010; Johnson,
1989).
So if we
really want to demonstrate psychosomatic effects, we've got to
get out of the nervous system, and into other systems of the
body -- like the gastrointestinal system, in the case of
psychosomatic ulcers. And
here's where hypnosis comes in, because we have a long history
of obtaining such effects with hypnosis (Black, 1969; Bowers & Kelly,
1979; Covino, 2008; Covino & Pinnell, 2010; Johnson,
1989).
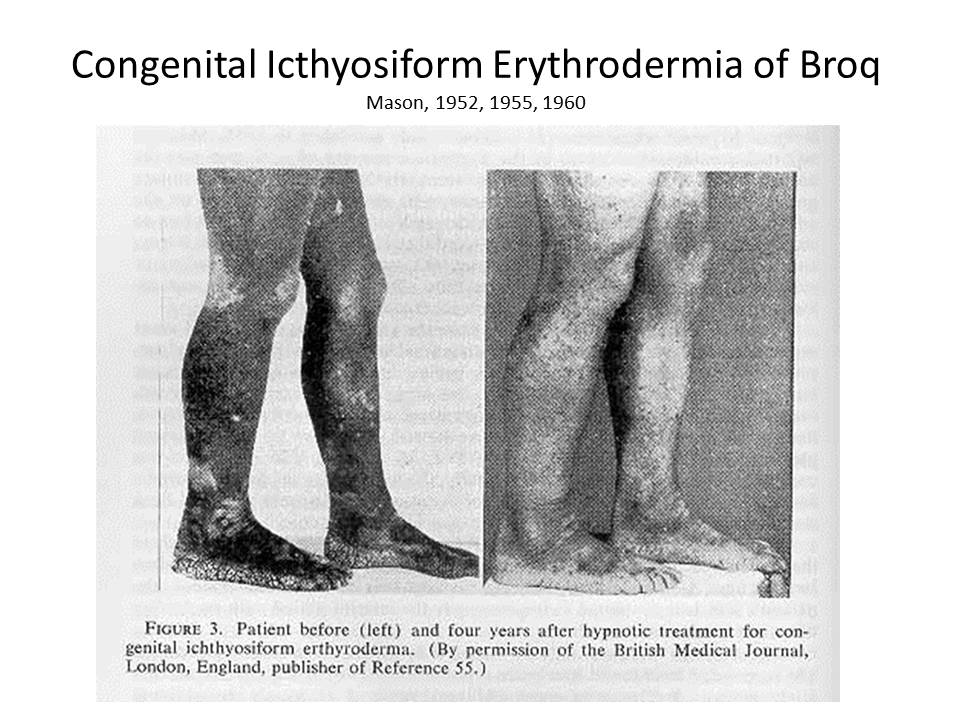 Perhaps the
"mother" of all such studies is the famous case, reported by
A.A. Mason, of a 16-year-old boy suffering from congenital
icthyosiform erythrodermia of Broq (Mason, 1952, 1955). This is a hereditary
disorder affecting the skin, which becomes discolored and
blackened, horny, inelastic, fissured, and peppered with
vascular protuberances. Conventional
treatment, including skin grafts from unaffected portions of
the body, failed. As
a last resort, Mason hypnotized the patient, and suggested
that the lesions would disappear -- first from one arm, then
the other, then the two legs each in turn, and finally the
trunk. The
progressive remission of the lesions, highly correlated with
the suggestions, was documented photographically both at the
end of treatment and at a four-year followup.
Perhaps the
"mother" of all such studies is the famous case, reported by
A.A. Mason, of a 16-year-old boy suffering from congenital
icthyosiform erythrodermia of Broq (Mason, 1952, 1955). This is a hereditary
disorder affecting the skin, which becomes discolored and
blackened, horny, inelastic, fissured, and peppered with
vascular protuberances. Conventional
treatment, including skin grafts from unaffected portions of
the body, failed. As
a last resort, Mason hypnotized the patient, and suggested
that the lesions would disappear -- first from one arm, then
the other, then the two legs each in turn, and finally the
trunk. The
progressive remission of the lesions, highly correlated with
the suggestions, was documented photographically both at the
end of treatment and at a four-year followup.
At these meetings in 2007, Mason reported that he subsequently
saw eight more cases like this, and hypnosis didn't work with
any of them. But
positive results have been obtained in other conditions. Just a couple of
highlights: these are mostly old studies, but they are very
provocative, so let me remind you of some of this history.
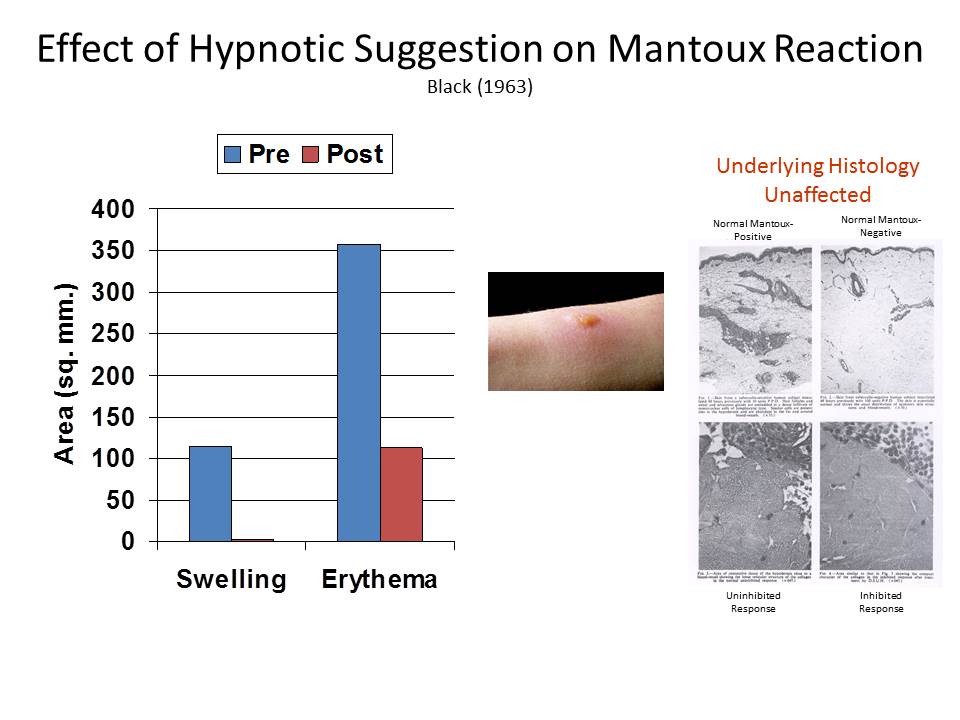 Some
of these cases involved the Mantoux reaction, a diagnostic
skin test for tuberculosis.
In another classic of the hypnosis literature, Stephen
Black gave four Mantoux-positive patients, all of whom were
known to be highly hypnotizable, suggestion decreased the size
of both the swelling and the hardened area (Black, Humphrey, & Niven,
1963). Interestingly,
a biopsy showed that the underlying histology was unchanged;
but, objectively, the swelling and hardness did go down.
Some
of these cases involved the Mantoux reaction, a diagnostic
skin test for tuberculosis.
In another classic of the hypnosis literature, Stephen
Black gave four Mantoux-positive patients, all of whom were
known to be highly hypnotizable, suggestion decreased the size
of both the swelling and the hardened area (Black, Humphrey, & Niven,
1963). Interestingly,
a biopsy showed that the underlying histology was unchanged;
but, objectively, the swelling and hardness did go down.
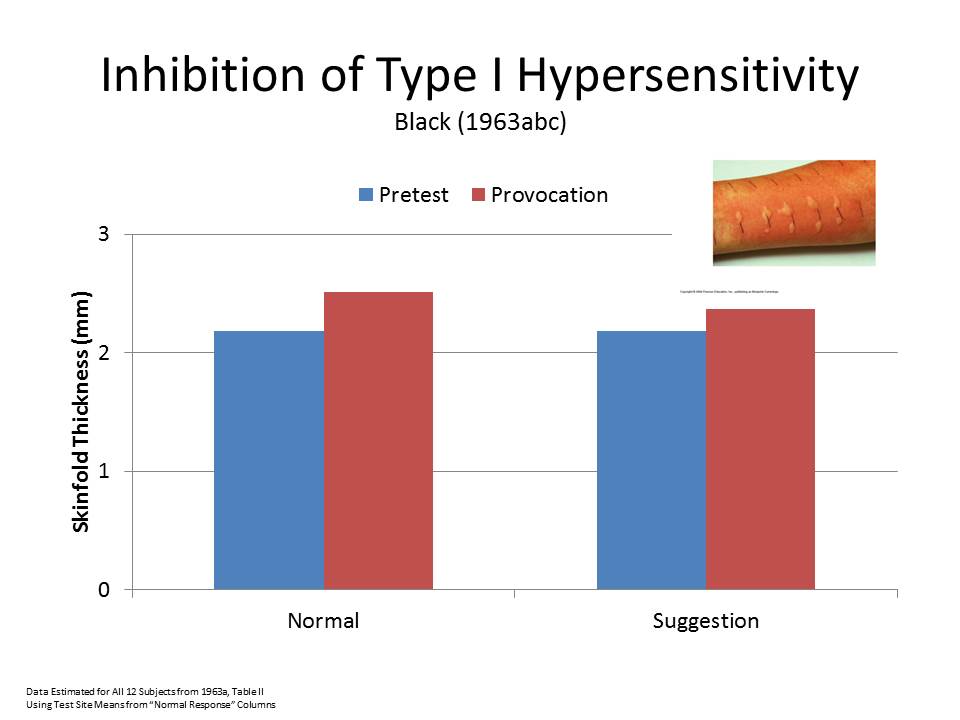 There have also been
positive results with allergic reactions. In one case of a
pollen allergy that had resisted treatment for 10 years, Mason
and Black found
that, after suggestion, the patient showed no hypersensitivity
to injected allergens (Mason
& Black, 1958). In a followup, Black tested
12 more patients, and obtained positive results with six of
the seven who were highly hypnotizable, and two of four who
were moderately hypnotizable (Black,
1963). Much
as with the Mantoux study, however, while the skin reaction
was inhibited, the Prausnitz-Kustner reaction indicated that
the underlying serology was unchanged.
There have also been
positive results with allergic reactions. In one case of a
pollen allergy that had resisted treatment for 10 years, Mason
and Black found
that, after suggestion, the patient showed no hypersensitivity
to injected allergens (Mason
& Black, 1958). In a followup, Black tested
12 more patients, and obtained positive results with six of
the seven who were highly hypnotizable, and two of four who
were moderately hypnotizable (Black,
1963). Much
as with the Mantoux study, however, while the skin reaction
was inhibited, the Prausnitz-Kustner reaction indicated that
the underlying serology was unchanged.
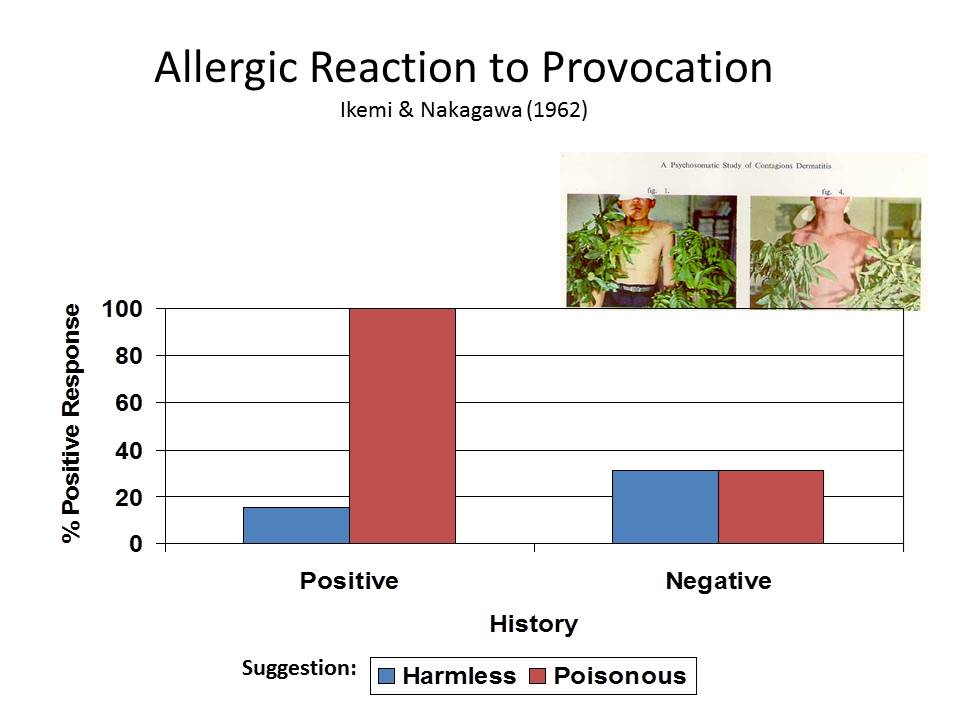 In yet
another classic study, Yujiro Ikemi and Shunji Nakagawa
employed a variant on the symptom-provocation method to study
the effects of suggestion on a form of contact dermatitis,
similar to poison ivy or poison oak, induced by skin contact
with the leaves of the lacquer and wax trees common in Japan
and other parts of East Asia (Ikemi
& Nakagawa, 1962).
In their study, 13 male high-school students, known to
be sensitive to these leaves, were blindfolded. When they were
actually brushed with the poisonous leaves, but told the
leaves were from the harmless chestnut tree, 11 subjects
showed reduced signs of dermatitis. When they were
touched with the chestnut-tree leaves, but told they were
being touched with poisonous leaves, all 13 showed signs of
dermatitis. When
the same procedure was applied to another group of students,
who had never experienced an allergic reaction to the
poisonous trees, there was little response to the suggestions
either way.
In yet
another classic study, Yujiro Ikemi and Shunji Nakagawa
employed a variant on the symptom-provocation method to study
the effects of suggestion on a form of contact dermatitis,
similar to poison ivy or poison oak, induced by skin contact
with the leaves of the lacquer and wax trees common in Japan
and other parts of East Asia (Ikemi
& Nakagawa, 1962).
In their study, 13 male high-school students, known to
be sensitive to these leaves, were blindfolded. When they were
actually brushed with the poisonous leaves, but told the
leaves were from the harmless chestnut tree, 11 subjects
showed reduced signs of dermatitis. When they were
touched with the chestnut-tree leaves, but told they were
being touched with poisonous leaves, all 13 showed signs of
dermatitis. When
the same procedure was applied to another group of students,
who had never experienced an allergic reaction to the
poisonous trees, there was little response to the suggestions
either way.
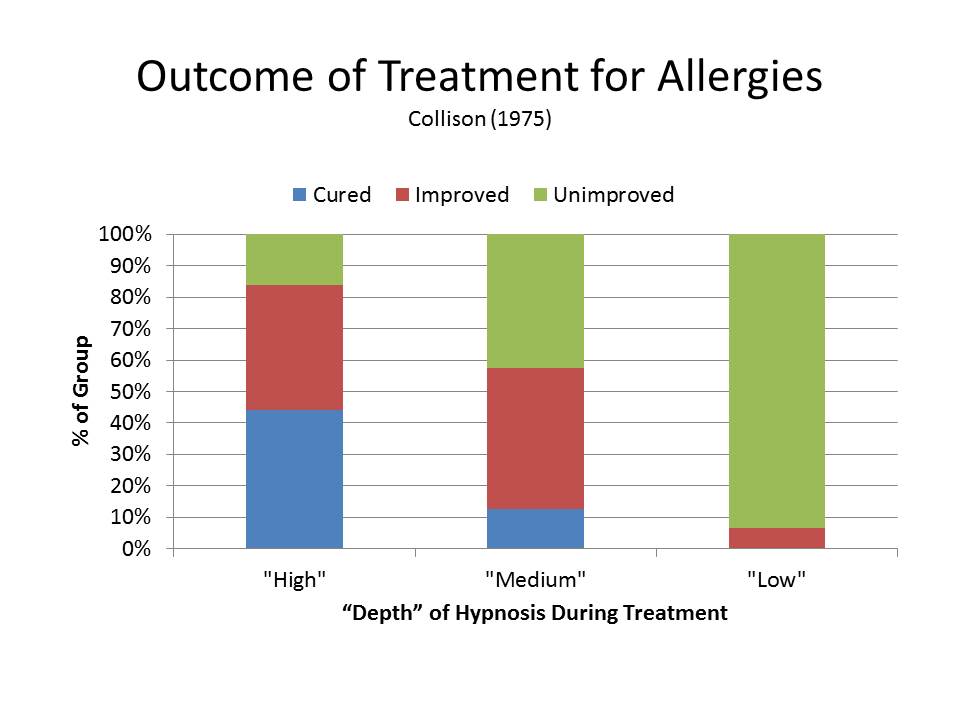 Finally, a
clinical series by David Collison (1975) included a large
number of allergic patients seen over a 10-year period. Dr. Collision did
not use a formal measure of hypnotizability, but he did make a
clinical assessment of the "depth" of hypnosis his patients
attained during treatment, which for my purposes can serve as
a proxy for hypnotizability.
Fully 19 of 43 hypnotizable patients showed complete
remission, and another 17 improved; six of 47 mediums were
cured, and only 21 improved; none of 31 insusceptible patients
were cured, though two did show improvement following
suggestion.
Finally, a
clinical series by David Collison (1975) included a large
number of allergic patients seen over a 10-year period. Dr. Collision did
not use a formal measure of hypnotizability, but he did make a
clinical assessment of the "depth" of hypnosis his patients
attained during treatment, which for my purposes can serve as
a proxy for hypnotizability.
Fully 19 of 43 hypnotizable patients showed complete
remission, and another 17 improved; six of 47 mediums were
cured, and only 21 improved; none of 31 insusceptible patients
were cured, though two did show improvement following
suggestion.
All of these are clinical studies, and lack the kind of
experimental controls that we'd need to really pin down these
effects. We'd
like to see better assessments of hypnotizability, for
example, and we'd also like to see a placebo condition. I say this because
some theorists seem inclined to identify the effects of
hypnosis with placebo effects.
This is a mistake on at least two counts. First, as I
indicated earlier, placebo effects are things that many
clinicians (and researchers) want to get rid of, and we don't
want to throw the hypnotic baby out with the placebic
bathwater. Second,
identifying hypnosis with placebos obscures the fact that
hypnosis is, itself, an active therapeutic agent -- just like
a drug or a pacemaker, surgery or psychotherapy. This is true even in
the case of pain, where placebo effects are arguably the
strongest (Evans &
McGlashan, 1987; McGlashan, Evans, & Orne, 1969).
In recent correspondence, Dr. Dabney Ewin has reminded me that
Mason's case of icthyosis was originally misdiagnosed as a
particularly bad one of warts.
And, in fact, it was this initial misdiagnosis that led
Mason to try hypnosis in the first place. He knew that
hypnosis had a long history as an effective treatment for
warts, so he gave it a shot.
If he had known that the patient's disease was
hereditary, he might never even have tried. So let's look at
hypnosis and warts for a moment.
The first such study to come to mind, of course, is Dr.
Ewin's own report of success in 80% of 41 consecutive cases (Ewin, 1992). Of course, warts
also remit spontaneously, so we'd like to see some additional
controls.
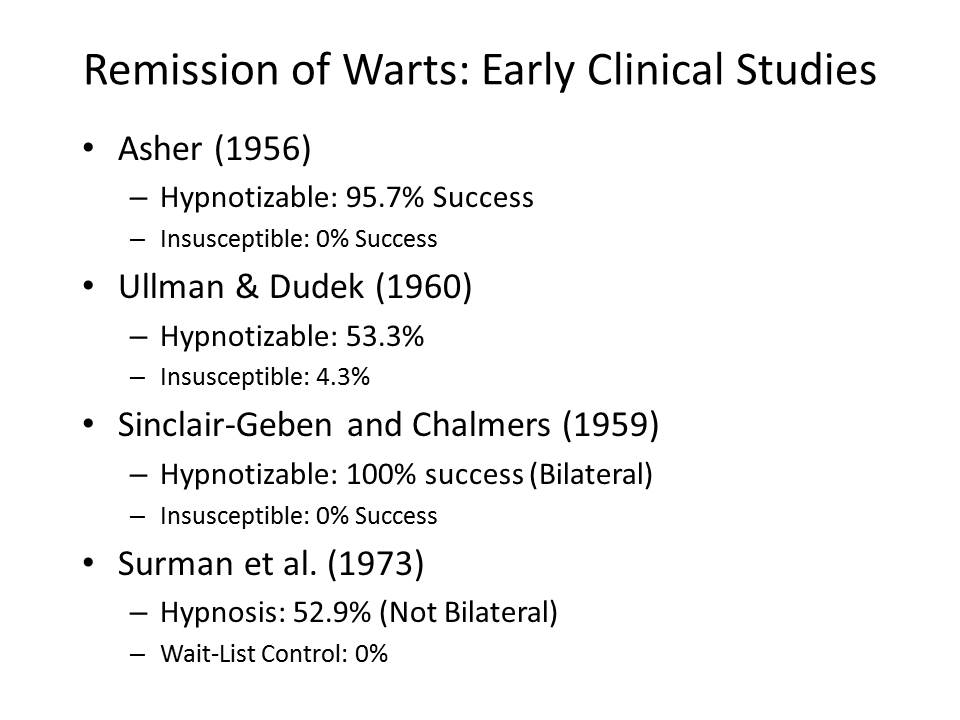 In a pioneering study, Asher
(1956) reported the results of 33 consecutive patients treated
for multiple warts, with cures in 11 of 17 hypnotizable
patients but none of 8 insusceptible patients. Ullman and Dudek got
a similar, if less dramatic difference between hypnotizable
and insusceptible patients, so there's something going on here
besides mere spontaneous regression. Sinclair-Gieben and
Chalmers (1959) treated 14 patients with bilateral warts with
hypnotic suggestions that targeted only one side of the body. On 3-month followup,
all 9 hypnotizable patients showed remission of the warts, but
only on the targeted side of the body; the 5 insusceptible
subjects showed no changes on either side. Again, this study
has a nice control for spontaneous remission: the untreated
side. Unfortunately,
a replication by Surman and colleagues found no difference
between treated and untreated sides, although they did report
some improvement in 9 of 17 patients given suggestions,
compared to none of 7 patients in an untreated wait-list
control condition (Surman,
Gottlieb, Hackett, & Silverberg, 1973).
In a pioneering study, Asher
(1956) reported the results of 33 consecutive patients treated
for multiple warts, with cures in 11 of 17 hypnotizable
patients but none of 8 insusceptible patients. Ullman and Dudek got
a similar, if less dramatic difference between hypnotizable
and insusceptible patients, so there's something going on here
besides mere spontaneous regression. Sinclair-Gieben and
Chalmers (1959) treated 14 patients with bilateral warts with
hypnotic suggestions that targeted only one side of the body. On 3-month followup,
all 9 hypnotizable patients showed remission of the warts, but
only on the targeted side of the body; the 5 insusceptible
subjects showed no changes on either side. Again, this study
has a nice control for spontaneous remission: the untreated
side. Unfortunately,
a replication by Surman and colleagues found no difference
between treated and untreated sides, although they did report
some improvement in 9 of 17 patients given suggestions,
compared to none of 7 patients in an untreated wait-list
control condition (Surman,
Gottlieb, Hackett, & Silverberg, 1973).
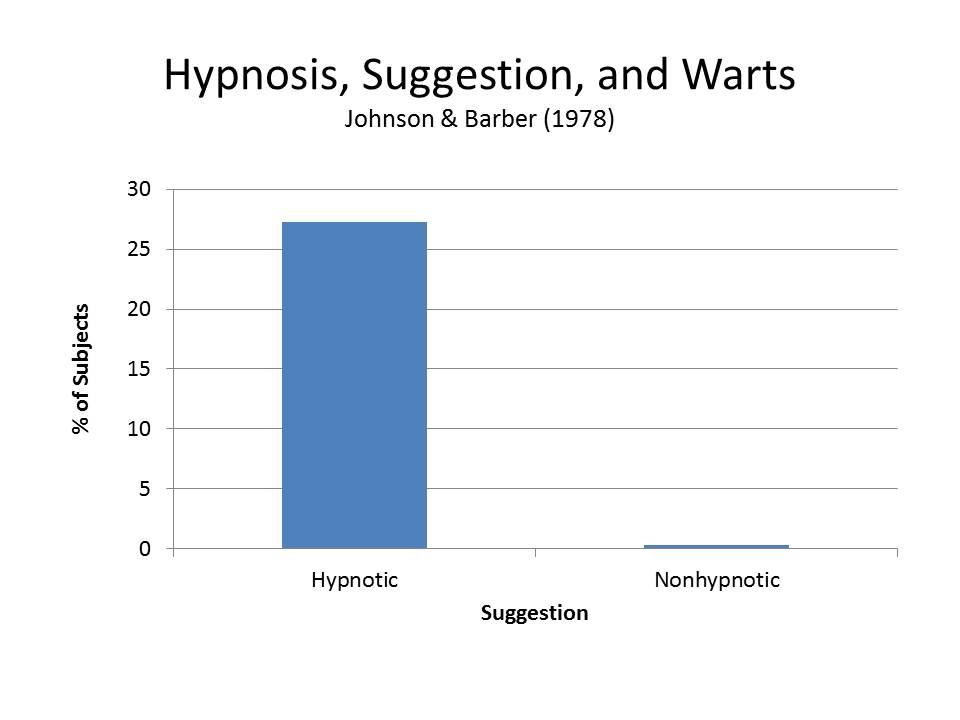 The first
investigators to bring this problem into the laboratory were
Richard Johnson and Ted Barber, who got a markedly lower
success rate: only 3 of 11 subjects given hypnotic suggestions
showed remission of their warts. But then again, none of the
11 subjects given the same suggestions without hypnosis showed
any improvement at all (Johnson,
1989). It's
unfortunate that Johnson and Barber didn't classify their
subjects according to hypnotizability -- though not
particularly surprising, given Barber's theoretical
orientation at the time In
fact, I believe that it was this study that prompted a turn in
Ted's theorizing, toward a view that hypnosis might have some
special properties after all (Barber,
1999, 2000).
The first
investigators to bring this problem into the laboratory were
Richard Johnson and Ted Barber, who got a markedly lower
success rate: only 3 of 11 subjects given hypnotic suggestions
showed remission of their warts. But then again, none of the
11 subjects given the same suggestions without hypnosis showed
any improvement at all (Johnson,
1989). It's
unfortunate that Johnson and Barber didn't classify their
subjects according to hypnotizability -- though not
particularly surprising, given Barber's theoretical
orientation at the time In
fact, I believe that it was this study that prompted a turn in
Ted's theorizing, toward a view that hypnosis might have some
special properties after all (Barber,
1999, 2000).
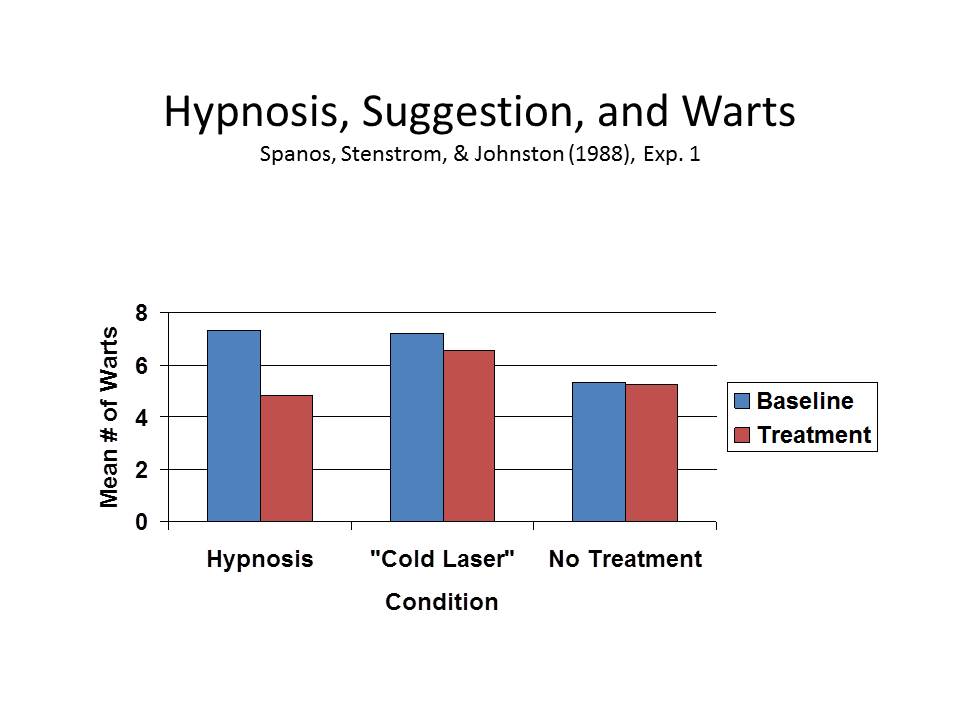 Nick Spanos
and his colleagues also attacked the problem of warts, and
with results that must have surprised them, too (Spanos, Stenstrom, & Johnson,
1988). Reasoning
that hypnosis might work by virtue of the myths and urban
legends surrounding it, they included a plausible placebo
control in the form of a "cold laser" machine for wart
removal, as well as an untreated control group. Only hypnosis led to
a significant reduction in warts.
Nick Spanos
and his colleagues also attacked the problem of warts, and
with results that must have surprised them, too (Spanos, Stenstrom, & Johnson,
1988). Reasoning
that hypnosis might work by virtue of the myths and urban
legends surrounding it, they included a plausible placebo
control in the form of a "cold laser" machine for wart
removal, as well as an untreated control group. Only hypnosis led to
a significant reduction in warts.
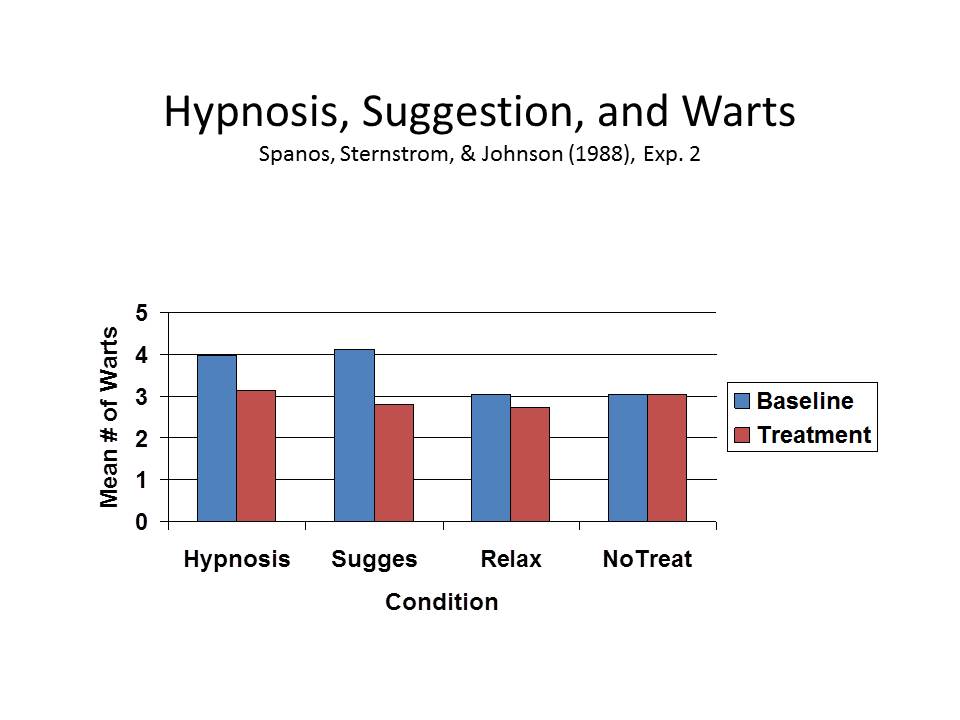 A second
study employed four groups, and got comparable effects when
subjects received a nonhypnotic suggestion, leading the
authors to conclude that the operative factor was the
suggestion, not hypnosis -- a point to which I'll return
later.
A second
study employed four groups, and got comparable effects when
subjects received a nonhypnotic suggestion, leading the
authors to conclude that the operative factor was the
suggestion, not hypnosis -- a point to which I'll return
later.
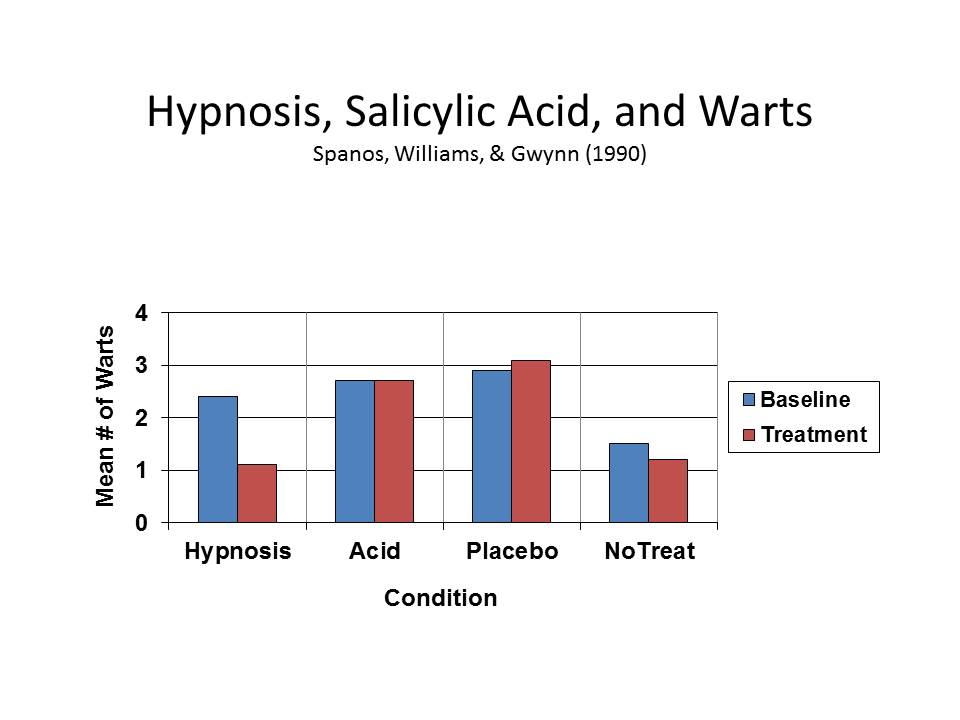 In a later study, hypnosis
proved superior to a common over-the-counter medical
treatment, the topical application of salicylic acid, as well
as a topical placebo (Spanos,
Williams, & Gwynn, 1990). It would be very
interesting to see a similar study comparing hypnosis with
liquid nitrogen cryotherapy, which is the current standard of
care.
In a later study, hypnosis
proved superior to a common over-the-counter medical
treatment, the topical application of salicylic acid, as well
as a topical placebo (Spanos,
Williams, & Gwynn, 1990). It would be very
interesting to see a similar study comparing hypnosis with
liquid nitrogen cryotherapy, which is the current standard of
care.
There are lots more studies of
warts, but the ones that I've cited make the point
convincingly: there just might be something interesting going
on here: the hypnotist's suggestion is having an effect on a
physiological process that lies outside the brain and central
nervous system. Note,
too, that these studies arise, first, in the clinic -- and
then are brought into the laboratory for systematic controlled
investigation. There
are a still a lot of questions that have to be answered. To illustrate, let's
follow the warts example a little further.
 First, of course, we need to
nail down any effects definitively, by including placebo and
untreated control groups -- and, for that matter, comparisons
to the standard of care.
It may be, for example, that hypnosis can't match the
outcomes achieved with the standard of care -- whether that is
salicylic acid or liquid nitrogen. But it might be
useful when, for whatever reason, the standard medical
treatment is inappropriate.
First, of course, we need to
nail down any effects definitively, by including placebo and
untreated control groups -- and, for that matter, comparisons
to the standard of care.
It may be, for example, that hypnosis can't match the
outcomes achieved with the standard of care -- whether that is
salicylic acid or liquid nitrogen. But it might be
useful when, for whatever reason, the standard medical
treatment is inappropriate.
At the same time, the combination of
hypnosis with the standard of care may be particularly
effective -- much as the combination of drugs with
psychotherapy is particularly potent with depression. Alternatively,
it may be that standard medical treatment is better at
immediate symptom relief, but hypnosis is better at
maintaining remission. Liquid
nitrogen might get rid of warts fairly quickly, but hypnosis
might keep them away.
We need clarification on the role of hypnotizability in
moderating these effects.
By definition, any effect of hypnosis ought to be
correlated with hypnotizability.
There are hints in the clinical studies of warts that
this might be the case -- though, unfortunately, the
laboratory studies failed to classify subjects for
hypnotizability.
On the other hand, we should also compare hypnosis with
nonhypnotic suggestion. In
one of his studies, Spanos got comparable effects without
inducing hypnosis. Here
again, hypnotizability may be an issue. In the case of skin
allergy, for example, Ikema and Nakazawa got their effects
regardless of whether they used hypnosis -- so long as the
subjects themselves were hypnotizable.
Then we need to know how "deep" these effects go. None of the warts
studies have done anything more than count the number of warts
visible before and after treatment. But warts are caused
by one or another form of the human papilloma virus (HPV):
there may be hundreds of these, though apparently only a small
number are clinically important.
We'd like to know whether there are effects on the HPV
virus itself. Recall
that, in his studies, Black found that hypnotic suggestion
modified the expression of the Mantoux reaction on the surface
of the skin, but not the underlying histology. On the other hand,
his suggestion didn't target the underlying histology -- only the visible surface
of the skin.
And how broad are these effects?
Most studies of warts target common cutaneous warts,
caused by HPV Types 2 and 4, which are benign if annoying. But what about the
more troublesome plantar warts, which are caused by a
different strain of HPV, Type 1?
Or something more serious, like genital warts, caused
by HPV 6 and 11? Even
in this age of Gardasil, there are as many as a million new
cases of genital each year.
Can we get rid of those warts as well? Can we prevent them
from coming back? What
are the effects of hypnotic treatment on the risk for cervical
cancer?
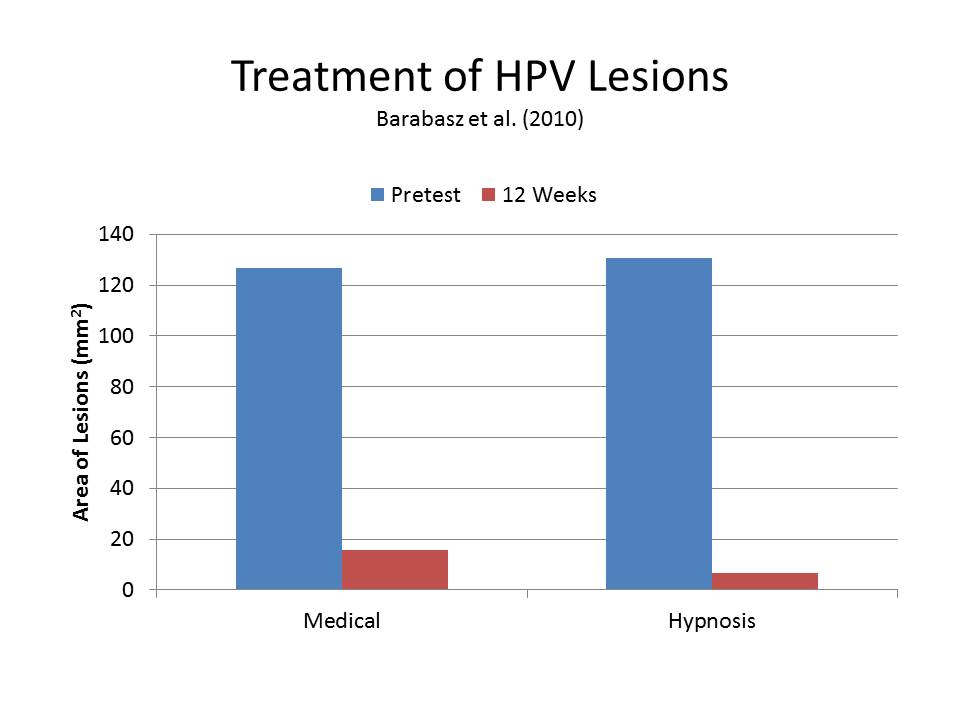 In
this regard, Arreed and Marianne Barabasz and their colleagues
published a very promising study comparing hypnosis with
standard medical treatments, which included topical Imiquimod
(which is directed at the immune response), cryotherapy, or
surgical removal (Barabasz,
Higley, Christensen, & Barabasz, 2010). The study did not
employ random assignment to conditions, but even so hypnosis
did as well as conventional treatment, even at 12-week
followup.
In
this regard, Arreed and Marianne Barabasz and their colleagues
published a very promising study comparing hypnosis with
standard medical treatments, which included topical Imiquimod
(which is directed at the immune response), cryotherapy, or
surgical removal (Barabasz,
Higley, Christensen, & Barabasz, 2010). The study did not
employ random assignment to conditions, but even so hypnosis
did as well as conventional treatment, even at 12-week
followup.
This is an area of research in which clinicians and
experimentalists can collaborate as equals, in a way that
benefits both constituencies.
In some respects, our clinical colleagues are way ahead
of the experimentalists -- trying hypnosis to see whether it
works. On the
other hand, controlled laboratory research will promote
clinical utilization, by giving skeptical colleagues a reason
to try hypnosis for themselves -- and third parties a reason
to pay for it.
 One area of potential
application, relatively unstudied, is burns (Patterson, Goldberg, & Ehde,
1996). Again,
I think of Dabney Ewin's remarkable case study of a boy who
was burned by boiling cooking fat (Ewin, 1986). And there are some
controlled experiments, too, which raise further questions
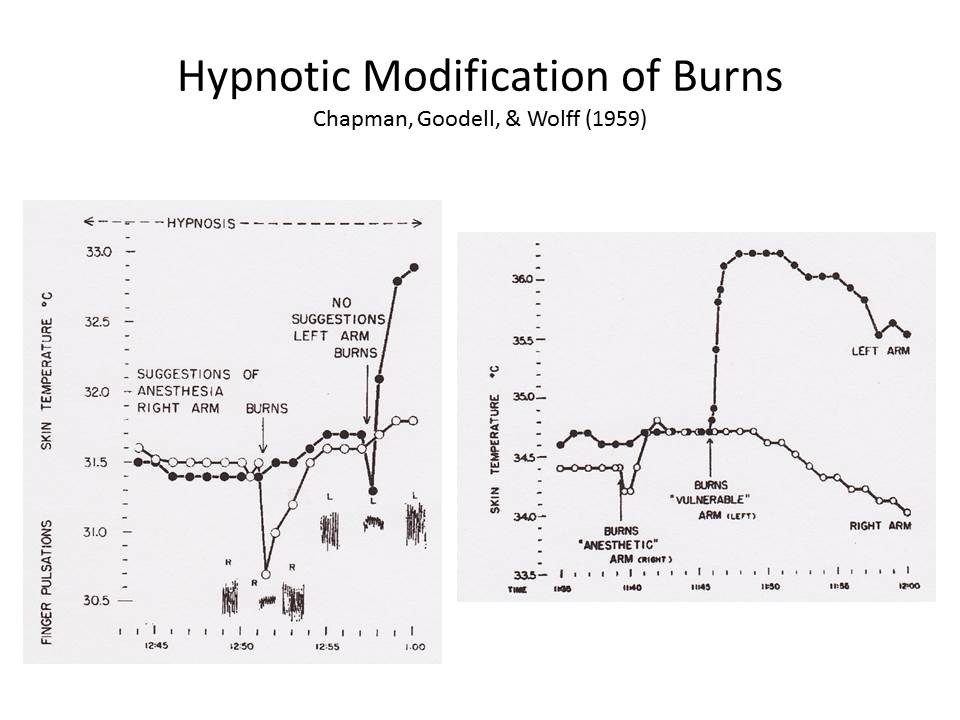
about the mechanics of these effects. In a classic study,
Chapman, Goodell, and Wolff found that targeted suggestions
decreased inflammation in experimentally induced bilateral
burns (Chapman, Goodell, &
Wolff, 1959a, 1959b).
They also found that the suggestion of a burn
increased skin temperature (Hammond,
Keye, & Grant, 1983). There are also some
clinical studies, which raise additional questions of
mechanism (Margolis, Domangue,
Ehleben, & Shrier, 1983; Moore & Kaplan, 1983). For example, how
much of the healing is a side effect of suggested analgesia? What are the effects
of suggestions for cooling of the skin in the affected area,
or increased blood flow?
One area of potential
application, relatively unstudied, is burns (Patterson, Goldberg, & Ehde,
1996). Again,
I think of Dabney Ewin's remarkable case study of a boy who
was burned by boiling cooking fat (Ewin, 1986). And there are some
controlled experiments, too, which raise further questions
about the mechanics of these effects. In a classic study,
Chapman, Goodell, and Wolff found that targeted suggestions
decreased inflammation in experimentally induced bilateral
burns (Chapman, Goodell, &
Wolff, 1959a, 1959b).
They also found that the suggestion of a burn
increased skin temperature (Hammond,
Keye, & Grant, 1983). There are also some
clinical studies, which raise additional questions of
mechanism (Margolis, Domangue,
Ehleben, & Shrier, 1983; Moore & Kaplan, 1983). For example, how
much of the healing is a side effect of suggested analgesia? What are the effects
of suggestions for cooling of the skin in the affected area,
or increased blood flow?
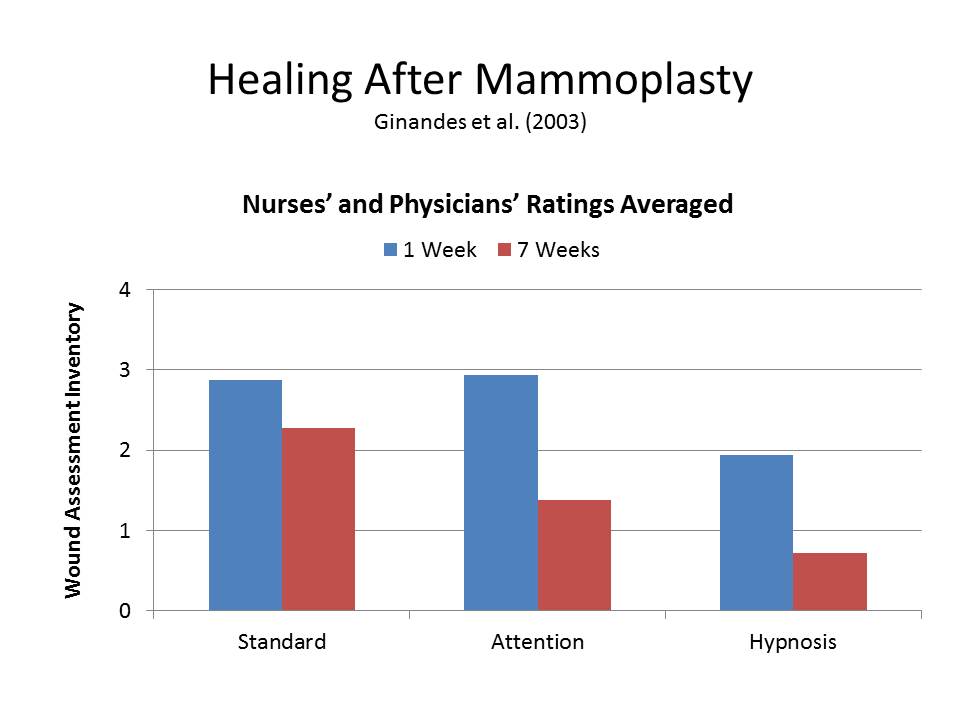 Similar studies could be
done in the area of wound-healing, whether the wounds are
surgically induced or a product of misadventure. Ginandes and her
colleagues found that adjunctive hypnosis accelerated healing
after reduction mammoplasty (Ginandes,
Brooks, Sando, Jones, & Aker, 2003). Compared to a group
who received the surgical standard of care, patients who
received adjunctive hypnosis showed faster wound healing over
7 weeks post-surgery. These
same authors had earlier found similar effects on the healing
of bone fractures, which offers another area for clinical
research (Ginandes &
Rosenthal., 1999).
Again, we'd like to know how much of these effects are
due to direct suggestion, and how much to relaxation and
stress-reduction.
Similar studies could be
done in the area of wound-healing, whether the wounds are
surgically induced or a product of misadventure. Ginandes and her
colleagues found that adjunctive hypnosis accelerated healing
after reduction mammoplasty (Ginandes,
Brooks, Sando, Jones, & Aker, 2003). Compared to a group
who received the surgical standard of care, patients who
received adjunctive hypnosis showed faster wound healing over
7 weeks post-surgery. These
same authors had earlier found similar effects on the healing
of bone fractures, which offers another area for clinical
research (Ginandes &
Rosenthal., 1999).
Again, we'd like to know how much of these effects are
due to direct suggestion, and how much to relaxation and
stress-reduction.
There are many more
studies along these lines.
Most of them are old, many of them are small in scope,
and some do not come up to contemporary standards for either
clinical or experimental research. But I've reviewed
them here because they constitute a legacy of hypnosis that
has been largely forgotten or ignored -- a legacy that still
holds considerable potential value for both clinical practice
and basic theory.
 On
the practical side, they suggest that hypnosis has the
potential to be an important treatment modality in a wide
variety of medical contexts -- not just in psychotherapy, or
for the relief of pain. Now,
I don't want to oversell these effects. Nobody treating
cancer should abandon surgery, radiation, or chemotherapy in
favor of hypnosis. But
it seems likely that hypnosis has a place in the active
treatment of a wide variety of medical conditions, especially
as an adjunct to standard medical treatments. The use of hypnosis
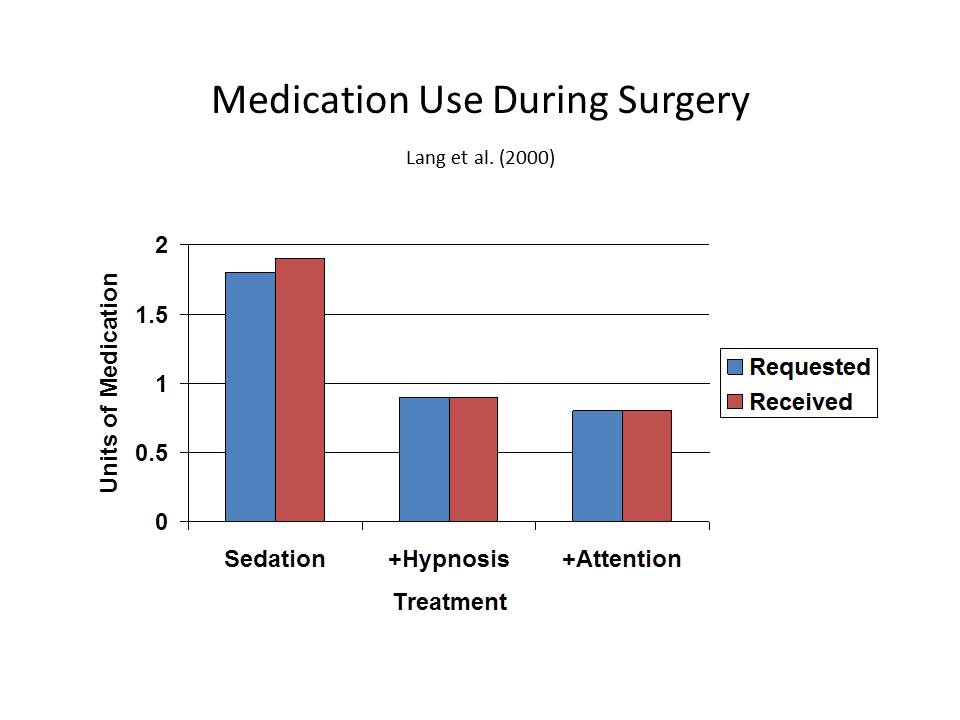
in the pain clinic may be a model here. For example, Elvira
Lang and her associates have shown clearly that adjunctive
hypnosis can reduce requests for conscious sedation in
outpatient surgery, and it's cost-effective as well! (Lang et al., 2000). (A distraction
condition also reduced medication use, but hypnosis had other
advantages that aren't shown here.) More results like
that should enhance the appeal of hypnosis to both service
providers and third-party payers.
On
the practical side, they suggest that hypnosis has the
potential to be an important treatment modality in a wide
variety of medical contexts -- not just in psychotherapy, or
for the relief of pain. Now,
I don't want to oversell these effects. Nobody treating
cancer should abandon surgery, radiation, or chemotherapy in
favor of hypnosis. But
it seems likely that hypnosis has a place in the active
treatment of a wide variety of medical conditions, especially
as an adjunct to standard medical treatments. The use of hypnosis
in the pain clinic may be a model here. For example, Elvira
Lang and her associates have shown clearly that adjunctive
hypnosis can reduce requests for conscious sedation in
outpatient surgery, and it's cost-effective as well! (Lang et al., 2000). (A distraction
condition also reduced medication use, but hypnosis had other
advantages that aren't shown here.) More results like
that should enhance the appeal of hypnosis to both service
providers and third-party payers.
 But even if the effects of
hypnosis on bodily functions are not substantial or reliable
enough to be of routine clinical use, they're still of great
potential theoretical importance, because of their relevance
to the mind-body problem -- that great unsolved problem in
philosophy and psychology.
There are, actually four mind-body problems,
quite different from each other.
But even if the effects of
hypnosis on bodily functions are not substantial or reliable
enough to be of routine clinical use, they're still of great
potential theoretical importance, because of their relevance
to the mind-body problem -- that great unsolved problem in
philosophy and psychology.
There are, actually four mind-body problems,
quite different from each other.
First, there is the standard
mind-body problem, which has to do with the biological
substrates of mental life.
Here we are dealing with the neural correlates of
consciousness -- the causal link between brain states and
mental states. What
is going on in the brain when we perceive an object, remember
an event, or contemplate an idea? What are the neural
differences between conscious and unconscious perception, memory, and thought? And also the problem
of embodied cognition
-- how do other bodily states, such as those involved in
emotion and motivation, affect perception, memory, and
thought?
Second, there is the question of body without mind -- perhaps
bringing up images of Hollywood zombies, who lack conscious
awareness and control. How
much of our behavior occurs independently of any conscious
mental processes at all?
How much is just plain reflex or instinct? How much is
automatic, executed outside of conscious awareness and without
any conscious intention?
Third, the question of mind without body. Does mental life
exist in the absence of any physical substrate at all? In the 19th
century, this was the domain of spiritualism. In the 20th
and 21st centuries, we call it parapsychology, the
out-of-body experience, or the near-death experience.
And last, but not least, the problem that has been my topic
today: how mind influences body -- how beliefs, attitudes,
ideas, and other thoughts can influence bodily states and
processes. This
is the theoretical relevance of psychosomatics, and it is here
where hypnosis can make a great, I think unique, contribution,
because they take us beyond the stress-disease connection. It's one thing for
stress to cause disease through activation of the autonomic
nervous system, the HPA and SMA, and all that, as in the case
of cardiovascular disease, ulcers, and other conditions. It's one thing for
relaxation, meditation, and other stress-reduction techniques
to help reverse these stress-related conditions. It's quite another
thing for a patient's belief that he is in contact with a
poisonous plant leaf to give rise to an eruption of
dermatitis, or for a suggestion that warts will disappear to
lead to their actual disappearance.
Now, with further research it may turn out that hypnosis isn't
necessary to produce these effects, or even high
hypnotizability. It
doesn't really matter. We'd
never find out about these psychosomatic relationships except
for the inspiration that came from hypnosis research. In that way,
hypnosis will once again lead the way to discovering something
new about mind and body.
Thank
you very much. Welcome
to Berkeley, and have an enjoyable meeting.
References
Alexander,
F. (1950). Psychosomatic
medicine: Its principles and applications. New York:
Norton.
Barabasz,
A., Higley, L., Christensen, C., & Barabasz, M.
(2010). Efficacy of hypnosis in the tretament of human
papillomavirus (HPV) in women: Rural and urban samples. International
Journal of Clinical
& Experimental Hypnosis, 58(1), 102-121.
Barber,
T. X. (1999). Hypnosis: A mature view. Contemporary
Hypnosis, 16, 123-127.
Barber,
T. X. (2000). A deeper understanding of hypnosis: Its
secrets, its nature, its essence. AMERICAN JOURNAL OF
CLINICAL HYPNOSIS, 42(3-4), 208-272.
Beecher,
H. K. (1955). The powerful placebo. Journal of the
American Medical Association, 159, 1602-1606.
Black,
S. (1963). Inhibition of immediate-type hypersensitivity
response by direct suggestion under hypnosis. British Medical
Journal(June 22), 925.
Black,
s. (1969). Mind and
body. London: Kimber.
Black,
S., Humphrey, H. H., & Niven, J. S. F. (1963).
Inhibition of Mantoux Reaction by direct suggestion under
hypnosis. Brit.
med. J., 5346, 1649-1652.
Bowers,
K. S., & Kelly, P. (1979). Stress, disease,
psychotherapy, and hypnosis. Journal of Abnormal
Psychology, 88, 506-526.
Chapman,
L. F., Goodell, H., & Wolff, H. G. (1959a).
Augmentation of the inflammatory reaction by activity of
the central nervous system. AMA Archives of
Neurology, 1(5), 557-572.
Chapman,
L. F., Goodell, H., & Wolff, H. G. (1959b). Changes in
tissue vulnerability induced during hypnotic suggestion. Journal of
Psychosomatic Research, 4, 99-105.
Cohen,
S., Janicki-Deverts, D., & Miller, G. E. (2007).
Psychological stress and disease. Journal of the
American Medical Association, 298, 1685-1687.
Covino,
N. A. (2008). Medical illnesses, conditions and
procedures. In M. R. Nash & A. J. Barnier (Eds.), Oxford handbook of
hypnosis: Theory, research, and practice (pp.
611-624). Oxford: Oxford University Press.
Covino,
N. A., & Pinnell, C. M. (2010). Hypnosis and medicine.
In s. J. Lynn, J. W. Rhue & I. Kirsch (Eds.), Handbook of clinical
hypnosis (pp. 551-573). Washington, d.C.: American
Psychological Association.
Evans,
F. J. (1974). The placebo response in pain reduction. In
J. J. Bonica (Ed.), Advances in Neurology (pp. 289-296). New
York: Raven.
Evans,
F. J., & McGlashan, T. H. (1987). Specific and
nonspecific factors in hypnotic analgesia: A reply to
Wagstaff. British
Journal of Experimental and Clinical Hypnosis, 4,
141-147.
Ewin,
D. M. (1986). Emergency room hypnosis for the burned
patient. Americal
Journal of Clinical Hypnosis, 29, 7-12.
Ewin,
D. M. (1992). Hypnotherapy for warts (verruca-vulgaris):
41 consecutive cases with 33 cures. American Journal of
Clinical Hypnosis, 35, 1-10.
Flammer,
E., & Alladin, A. (2007). The efficacy of hypnotherapy
in the treatment of psychosomatic disorders:
Meta-analytical evidence. International Journal
of Clinical
& Experimental Hypnosis, 55(3), 251-274.
Ginandes,
C., Brooks, P., Sando, W., Jones, C., & Aker, J.
(2003). Can Medical Hypnosis Accelerate Post-Surgical
Wound Healing? Results of a Clinical Trial. American Journal of
Clinical Hypnosis, 45(4), 333-352.
Ginandes,
C., & Rosenthal., D. I. (1999). Using hypnosis to
accelerate the healing of bone fractures: A randomized
controlled pilot study. Altern Th H, 5, 67+.
Hammond,
D. C., Keye, W. R., & Grant, C. W. (1983). Hypnotic
analgesia with burns: An initial study. American Journal of
Clinical Hypnosis, 26, 60-61.
Harrington,
A. (2008). The cure
within: A history of mind-body medicine. N.Y.:
Norton.
Harrington,
A. (Ed.). (1997). The
placebo effect: An interdisciplinary exploration.
Cambridge, Ma.: Harvard University Press.
Healy,
D. (2004). The
creation of psychopharmacology. Cambridge, Ma.:
Harvard University Press.
Hilgard,
E. R. (1948). Theories
of learning. New York,: Appleton-Century-Crofts.
Hilgard,
E. R. (1952). Experimental approaches to psychoanalysis.
In E. Pumpian-Mindlin (Ed.), Psychoanalysis as
science: The Hixon Lectures on the scientific status of
psychoanalysis (pp. 3-45). Stanford, Ca.: Stanford
University Press.
Hilgard,
E. R. (1961). Hypnosis and experimental psychodynamics Lectures on
experimental psychiatry (pp. 193-212). Pittsburgh,
Pa.: University of Pittsburgh Press.
Hilgard,
E. R. (1977). Divided
consciousness: Multiple controls in human thought and
action. New York: Wiley-Interscience.
Hilgard,
E. R., & Marquis, D. G. (1940). Conditioning and
learning. New York, London,: D. Appleton-Century
Company.
Hrobjartsson,
A., & Gotzsche, P. C. (2001a). Core belief in powerful
effects of placebo interventions is in conflict with no
evidence of important effects in a large systematic
review. Advances in
Mind-Body Medicine, 17, 312-318.
Hrobjartsson,
A., & Gotzsche, P. C. (2001b). Is the placebo
powerless? An
analysis of clinical trials comparing placebo with no
treatment. New
England Journal of Medicine, 344(21), 1594-1602.
Hull,
C. L. (1929). Quantitative methods of investigating waking
suggestion. Journal
of Abnormal & Social Psychology, 24, 153-169.
Hull,
C. L. (1930a). Quantitative methods of investigating
hypnotic suggestion.
Part 1. Journal
of Abnormal & Social Psychology, 25, 200-223.
Hull,
C. L. (1930b). Quantitative methods of investigating
hypnotic suggestion.
Part 2. Journal
of Abnormal & Social Psychology, 25, 390-417.
Hull,
C. L. (1933). Hypnosis
and suggestibility: An experimental approach. New
York: Appleton.
Hyman,
S. E. (1994). Another one bites the dust: An infectious
origin for peptic ulcers. Harvard Review of
Psychiatry, 1, 294-295.
Ikemi,
Y., & Nakagawa, S. (1962). A psychosomatic study of
contagious dermatitis. Kyushu Journal of Medical Science, 13,
335-352ff.
nsel, T. R. (2010). Faulty circuits.
Scientific
American(April).
James,
W. (1890/1980). Principles
of Psychology. Cambridge, Ma.: Harvard University
Press.
Johnson,
R. F. Q. (1989). Hypnosis, suggestion, and dermatological
changesL A consideration of the production and diminution
of dermatological entities. In N. P. Spanos & J. F.
Chaves (Eds.), Hypnosis:
Cognitive-behavioral perspectives (pp. 297-312).
Buffalo, N.Y.: Prometheus.
Kihlstrom,
J. F. (1979). Hypnosis and psychopathology: Retrospect and
prospect. Journal
of Abnormal Psychology, 88(5), 459-473.
Kihlstrom,
J. F. (1994). One hundred years of hysteria. In S. J. Lynn
& J. W. Rhue (Eds.), Dissociation:
Clinical and theoretical perspectives. (pp.
365-394). New York, NY, USA: The Guilford Press.
Kihlstrom,
J. F. (2003). Expecting that a treatment will be given,
when it won't, and knowing that a treatment is being
given, when it is [Commentary on "Open versus hidden
medical treatments: The patient's knowledge about a
therapy affects therapy outcome" by F. Benedetti, G.
Maggi, L. Lopiano, M. Lanotte, I. Rainero, S. Vighetti,
& A Pollo]. Prevention
& Treatment, 6, Article 4.
Kihlstrom,
J. F. (2007). What
hypnosis does for experimental psychology. Paper
presented at the American Psychological Association, San
Francisico.
Kihlstrom,
J. F. (2008). Placebo: Feeling better, getting better, and
the problems of mind and body. McGill Journal of
Medicine, 11, 212-214.
Kihlstrom,
J. F. (2013). Hypnosis and cognition. Psychology of
Consciousness, submitted.
Kihlstrom,
J. F., & Canter Kihlstrom, L. (1999). Self, sickness,
somatization, and systems of care. In R. J. Contrada &
R. D. Ashmore (Eds.), Self, social identity, and physical health:
interdisciplinary explorations (Vol. 2). New York:
Oxford University Press.
Kihlstrom,
J. F., & McConkey, K. M. (1990). William James and
hypnosis: A centennial reflection. Psychological
Science, 1(3), 174-178.
Kirsch,
I., Moore, T. J., Scoboria, A., & Nicholls, S. S.
(2002). The emperor's new drugs: An analysis of
antidepressant medication data submitted to the US Food
and Drug Administration. Prevention &
Treatment, 5(Article 23).
Kosslyn,
S. M., Thompson, W. L., Costantini-Ferrando, M. F.,
Alpert, N. M., & Spiegel, D. (2000). Hypnotic visual
hallucination alters brain color processing. American Journal of
Psychiatry, 157(8), 1279-1284.
Lang, E. V., Benotsch, E. G., Fick, L. J., Lutgendorf, S.,
Berbaum, M. L., Berbaum, K. S., . . . Spiegel, D. (2000).
Adjunctive non-pharmacological analgesia for invasive
medical procedures: A randomised trial. Lancet, 355(April
29), 1486-1500.
Locke,
S. E., Ransil, B. J., Zachariae, R., Molay, F., Tollins,
K., Covino, N. A., & Danforth, D. (1994). Effect of
hypnotic suggestion on the delayed type hypersensitivity
response. Journal
of the American Medical Association, 272, 47-52.
Locke, S. E., Ransil, B. J., Covino, N. A., Toczydlo, J.,
Lohse, C. M., Dvorak, H. F., . . . Frankel, F. H. (1987).
Failure of hypnotic suggestion to alter immune response to
delayed type hypersensitivity antigens. Annals of the New
York Academy of Sciences, 496, 745-749.
Margolis,
c., Domangue, B. B., Ehleben, C., & Shrier, L. (1983).
Hypnosis in the early treatment of burns: A pilot study. American Journal of
Clinical Hypnosis, 26, 9-15.
Marshall,
B. J., & Warren, J. R. (1984). Unidentified curved
bacilli in the stomach of patients with gastritis and
peptic ulceration. Lancet,
1, 1311.
Mason,
A. A. (1952). A case of congenital ichthyosiform
erythrodermia of Broq treated by hypnosis. British medical
Journal(August 23), 422-423.
Mason,
A. A. (1955). Octhyosis and hypnosis. British medical
Journal(July 2), 57-58.
Mason,
A. A., & Black, S. (1958). Allergic skin responses
abolished under treatment of asthma and hayfever by
hypnosis. Lancet,
877-880.
McGlashan,
T. H., Evans, F. J., & Orne, M. T. (1969). The nature
of hypnotic analgesia and placebo resonse to expeimental
pain. Psychosomatic
Medicine, 31, 227-246.
Minsky,
M. (1987). The
society of mind. New York: Simon & Schuster.
Moore,
L. E., & Kaplan, J. Z. (1983). Hypnotically
accelerated burn wound healing. American Journal of
Clinical Hypnosis, 26(1), 16-19.
Neisser,
U. (1967). Cognitive
psychology. New York: Appleton-Century-Crofts.
Nomura,
A., Stemmermann, G. N., Chyou, P.-H., Perez-Perez, G. I.,
& Blaser, M. J. (1994). Helicobacter pylori infection
and the risk for duodenal and gastric ulceration. Annals of Internal
Medicine, 120, 977-981.
Overmier,
J. B., & Murison, R. (2013). Restoring psychology's
role in peptic ulcer. Applied Psychology:
Health & Well-Being, in press.
Patterson,
D. R., Goldberg, M. L., & Ehde, D. M. (1996). Hypnosis
in the treatment of patients with severe burns. American Journal of
Clinical Hypnosis, 38(3), 200-212; discussion 213.
Price,
D. D., Finniss, D. G., & Benedetti, F. (2008). A
comprehensive review of the placebo effect: recent
advances and current thought. Annual Review of
Psychology, 59, 565-590.
Rainville,
P., Hofbauer, R. K., Bushnell, M. C., Duncan, G. H., &
Price, D. D. (2002). Hypnosis modulates the activity in
cerebral structures involved in the regulation of
consciousness. Journal
of Cognitive Neuroscience, 14(Suppl), 887-901.
Shapiro,
A. K., & Shapiro, E. (1997). The powerful placebo:
From ancient priest to modern physician. Baltimore,
Md.: Johns Hopkins University press.
Spanos,
N. P., Stenstrom, R. J., & Johnson, J. C. (1988).
Hypnosis, placebo, and suggestion in the treatmet of
warts. Psychosomatic
Medicine, 50, 245-260.
Spanos,
N. P., Williams, V., & Gwynn, M. I. (1990). Effects of
hypnotic, placebo, and salicylic acid treatments on wart
regression. Psychosomatic
Medicine, 52, 109-114.
Surman,
O. S., Gottlieb, S. K., Hackett, T. P., & Silverberg,
E. L. (1973). Hypnosis in the treatment of warts. Archives of General
Psychiatry, 28, 439-441.
Young,
P. C. (1925). An experimental study of mental and physical
functions in the normal and hypnotic states. American Journal of
Psychology, 36, 214-232.
Young,
P. C. (1926a). An experimental study of mental and
physical functions in the normal and hypnotic states:
additional results. American
Journal of Psychology, 37, 345-356.
Young,
P. C. (1926b). Hypnotism. Psychological
Bulletin, 23(9), 504-523.
Young,
P. C. (1927). A general review of the literature of
hypnotism. Psychological
Bulletin, 24, 540-560.
Young,
P. C. (1931). A general review of the literature on
hypnotism and suggestion. Psychological
Bulletin, 28, 367-391.
This page last revised
10/02/2013.