The purpose of general anesthesia is to render surgical patients unconscious, and thus insensitive to pain and oblivious to events occurring during the procedure. For this reason, anesthesia -- like sleep and coma -- often enters into philosophical and scientific discussions of consciousness. How do we know that the patient is unconscious? Appearances to the contrary notwithstanding, are there reasons to think that anesthetized patients are actually conscious after all? Assuming that they are actually unconscious, is it possible for them to acquire and retain unconscious memories of pain and surgical events? What can the biological mechanisms of general anesthesia tell us about the neural correlates of consciousness?
Up until the middle of the 19th century, anesthesia was not a feature of surgery. Instead, patients were simply required to withstand the pain of the procedure, perhaps with the aid of alcohol, opiates (such as laudanum), a bite-board, and physical restraints.
In the early 1840s, James Elliotson and James Esdaille, two Scottish surgeons, successfully employed "Mesmerism", otherwise known as "animal magnetism", a forerunner to modern hypnosis, as an anesthetic agent in many surgical operations. Unfortunately, Mesmerism was in ill repute in scientific medicine. And their timing was bad: just as they were beginning to publish their results, the first chemical anesthetics were documented.
 Humphrey Davy (1778-1829), the pioneering electrochemist,
discovered the effects of nitrous oxide (first
synthesized by Joseph Priestly in 1772) on headache and dental
pain during his research on respiratory physiology; but his
report went unnoticed in the medical community and the
substance was quickly consigned to use at "laughing gas"
parties. The practice continues even in the present
time, with nitrous oxide offered as an intoxicant at raves and
music festivals like Burning Man (see "Nitrous Nation" by Ezra
Marcus, New York Times, 01/31/2021). According
to Klein, the recreational use of nitrous oxide gained
additional popularity as a response to social isolation during
the "lockdown" of the Covid-19 pandemic of 2020-2021.
Warning: Don't try this at home! While the death
rate from overdosing nitrous oxide is relatively low, but its
potential for psychological dependency, if not physiological
addiction, is relatively high. Nitrous oxide makes you
stupid, and stupid people can injure or kill themselves by
doing stupid things.
Humphrey Davy (1778-1829), the pioneering electrochemist,
discovered the effects of nitrous oxide (first
synthesized by Joseph Priestly in 1772) on headache and dental
pain during his research on respiratory physiology; but his
report went unnoticed in the medical community and the
substance was quickly consigned to use at "laughing gas"
parties. The practice continues even in the present
time, with nitrous oxide offered as an intoxicant at raves and
music festivals like Burning Man (see "Nitrous Nation" by Ezra
Marcus, New York Times, 01/31/2021). According
to Klein, the recreational use of nitrous oxide gained
additional popularity as a response to social isolation during
the "lockdown" of the Covid-19 pandemic of 2020-2021.
Warning: Don't try this at home! While the death
rate from overdosing nitrous oxide is relatively low, but its
potential for psychological dependency, if not physiological
addiction, is relatively high. Nitrous oxide makes you
stupid, and stupid people can injure or kill themselves by
doing stupid things.
In 1845, Horace Wells, an American dentist, successfully used nitrous oxide for anesthesia during a dental extraction. But when he attempted to repeat the demonstration before an audience of physicians and surgeons, the demonstration failed.
 But
But  on October 16, 1846, William
Morton, another dentist, employed ether in the
surgical removal of a tumor with no signs or reports of pain
in the patient. That event is now celebrated in hospitals and
medical schools throughout the world as "Ether Day". The
event is also immortalized in two
paintings: the one on the left,
by Robert Hinckley (1896), hangs in the
Countway Medical Library at Harvard Medical School; the
one on the right, by Warren and Lucia
Prosperi (2001), hangs in the "Ether Dome", the actual
surgical theatre -- complete with audience of physicians
and medical students -- where the operation took place.
on October 16, 1846, William
Morton, another dentist, employed ether in the
surgical removal of a tumor with no signs or reports of pain
in the patient. That event is now celebrated in hospitals and
medical schools throughout the world as "Ether Day". The
event is also immortalized in two
paintings: the one on the left,
by Robert Hinckley (1896), hangs in the
Countway Medical Library at Harvard Medical School; the
one on the right, by Warren and Lucia
Prosperi (2001), hangs in the "Ether Dome", the actual
surgical theatre -- complete with audience of physicians
and medical students -- where the operation took place.
Actually, ether had been used successfully for dental
anesthesia as early as 1842, and that same year Crawford Long,
a physician in Georgia, actually used ether in surgery.
However, in the 19th century dentistry wasn't considered
"real" medicine; and Long did not publish his results until
1849, so Morton got priority for his discovery (still, Morton
was a dentist; and Long had the major teaching hospital of
Emory University named for him!).
 Ether anesthesia
quickly crossed the Atlantic to England. In December
1846, William Squire and Robert Liston, surgeons at University
College, London, determined to see Morton's effects for
himself. Squire's uncle Peter, a pharmacist, had
fashioned an apparatus for delivering ether, consisting of a
glass flask attached to a mask with a rubber tube, and which
had already been used successfully for a dental extraction --
but then again, that was mere dentistry, not real
surgery. He coerced a hospital orderly to serve as
the demonstration subject, but the man was apparently bothered
by the ether fumes and ran from the surgical theatre.
Shortly thereafter, however, a real patient arrived: Frederick
Churchill, a butler with an infected leg that required
amputation. The surgery was performed with ether:
Churchill was completely unresponsive during the surgery; in
fact, when the ether wore off, he asked when the surgery was
going to begin. Lisiton announced to his audience of
physicians and medical students (another famous painting, "The
Agnew Clinic", by Thomas Eakins, at the Philadelphia Museum of
Art, also shows an anesthetist at work): "This Yankee dodge,
gentlemen, beats mesmerism hollow!".
Ether anesthesia
quickly crossed the Atlantic to England. In December
1846, William Squire and Robert Liston, surgeons at University
College, London, determined to see Morton's effects for
himself. Squire's uncle Peter, a pharmacist, had
fashioned an apparatus for delivering ether, consisting of a
glass flask attached to a mask with a rubber tube, and which
had already been used successfully for a dental extraction --
but then again, that was mere dentistry, not real
surgery. He coerced a hospital orderly to serve as
the demonstration subject, but the man was apparently bothered
by the ether fumes and ran from the surgical theatre.
Shortly thereafter, however, a real patient arrived: Frederick
Churchill, a butler with an infected leg that required
amputation. The surgery was performed with ether:
Churchill was completely unresponsive during the surgery; in
fact, when the ether wore off, he asked when the surgery was
going to begin. Lisiton announced to his audience of
physicians and medical students (another famous painting, "The
Agnew Clinic", by Thomas Eakins, at the Philadelphia Museum of
Art, also shows an anesthetist at work): "This Yankee dodge,
gentlemen, beats mesmerism hollow!".
A neat historical coincidence: one of the students in Liston's audience that day was Joseph Lister, who would go on to develop antiseptic methods for the control of infections secondary to surgical procedures (Listerine is named for him).
Morton died in 1868, and his tombstone in Cambridge's Mount Auburn Cemetery carries the following epitaph, composed by Bigelow:
Soon thereafter, in 1847, chloroform was
introduced by Simpson as an alternative to ether, which had
an unpleasant odor and other side effects.
Anesthesia was also extended from surgery to obstetrics,
although some physicians had qualms about dangers to the
neonate. Some religious authorities claimed that
anesthesia violated God's will that women give birth in pain
(see Genesis). Queen Victoria essentially
ended the debate in 1853 when she received chloroform for
the birth of her eighth (!) child, Prince Leopold. The first
American woman to give birth under chloroform was Fanny
Longfellow, wife of Henry Wadsworth Longfellow.
Nevertheless, some professionals and others continued to
debate a "calculus of suffering" by which some individuals,
and some conditions, were deemed more worthy of anesthesia
than others. And even in the 20th (and 21st) century,
the subjective nature of pain led both healthcare
professionals and political policymakers to disparage many
claims of "pain and suffering" as mere malingering.
For interesting histories of pain and pain control, see
- A Calculus of Suffering by Martin Pernick (1985).
- Pain: A Political History by Keith Wailoo (2014).
- Milk of Paradise: A History of Opium by Lucy Inglis (2018).
The story of Morton and Ether Day is told in "The Great Moment" (1944), a biopic directed by Preston Sturges.
The stories of Freud' and Halsted'
relationship to cocaine are told in two books:
Both books were reviewed by Frederick Crews in "Physician, Heal Thyself", published in two parts in the New York Review of Books (09/29/2011 and 10/13/2011).
Halsted became addicted during a program of self-experimentation on the anesthetic properties -- very common in medical research at the time. He managed to control his addiction, however, engaging in cocaine "binges" during vacations and other free time. More or less: Halsted was treated for his cocaine addiction with morphine (it was widely believed at the time that the two drugs were antagonists) -- and he promptly became a morphine enthusiast - -if not quite an addict -- as well.
Freud also experimented with cocaine in work
leading up to the publication of "On Coca" (Uber Coca,
1884), and other papers that, for some reason, didn't make
it into the Standard Edition of the Complete
Psychological Works of Sigmund Freud -- perhaps
because they were deemed "neurological" in nature.
In a reversal of Halsted's experience, but again based on
the belief that morphine and cocaine were physiological
antagonists, Freud advocated the use of cocaine for the
treatment of morphine addiction! Despite
Freud's advocacy, his principal case, his physician
colleague Ernst Fleischl, was a disaster.
Freud himself was not averse to the
recreational use of cocaine.
Ernest Jones, Freud's biographer (some would say hagiographer), dismisses the whole "cocaine episode" of 1884-1887 as an aberration. On the other hand, Crews, a vigorous critic of Freud and psychoanalysis, points out that the cocaine episode foreshadowed the problems with Freud's later psychotherapeutic work:
Already by 1886, then, Freud was displaying premature certainty, impatience with methodological safeguards, truculence, and a belief that he was destined for great things. Those weren't traits that blossomed after he developed psychoanalysis and felt a need to defend it. They were the very engine of invention.
***
At no point in either campaign did he place the safety and welfare of patients ahead of ambition. When cocaine was found to be tragically addictive for physicians and patients who had followed his thoughtless advise, he fought back desperately in 1887, bending the truth in order to exculpate himself. And when, after decades of claiming that psychoanalysis is the sovereign remedy for psychoneuroses, he allowed that he had "never been a therapeutic enthusiast", he didn't apologize; by then his fame as the Columbus of the unconscious was secure.
Freud's triumph in reaching that pinnacle without the aid of any confirmed discoveries or cures may be the most amazing chapter in the entire history of self-promotion.... Without cocaine, the polite and unhappy young doctor of April 1884 might never have become so reckless, so adamant, so sex preoccupied, and so convinced of his own importance that the contagion was caught by millions. Cocaine, along with nicotine, was Freud's drug of choice -- but in the century to come, the opiate of the educated classes would be psychoanalysis.
Throughout the 20th century, the techniques
for delivering and maintaining anesthesia were improved.
 Modern
anesthetic technique is known as balanced anesthesia,
because it employs a "cocktail" of different drugs to
achieve the goals of general anesthesia: sedation, loss of
consciousness (sometimes referred to as "narcosis" or
"hypnosis"), amnesia; and muscle relaxation.
Modern
anesthetic technique is known as balanced anesthesia,
because it employs a "cocktail" of different drugs to
achieve the goals of general anesthesia: sedation, loss of
consciousness (sometimes referred to as "narcosis" or
"hypnosis"), amnesia; and muscle relaxation.
There are also a number of alternatives to
general anesthesia:
There's even a turn toward no anesthesia
at all. That is, no general anesthesia, so that the
patient is wide awake during even major procedures that, in the past, would have involved general
anesthesia. In awake surgery
patients receive local or regional anesthesia to block pain, and conscious sedation to alleviate anxiety, but otherwise they're wide
awake during surgery, can watch the proceedings (though it's not clear
now much they'll remember, given
that they often receive
sedatives that are themselves amnestic agents),
and interact with the surgical team. Of
course, there are some downsides. The patient might
hear the surgeon comment on some problem encountered during
the procedure. Or, for that matter, the patient might
get bored and engage the anesthetist in
conversation. Medical students take courses in
doctor-patient communication, but, at
least until now, they've not been trained for anything
like this. Still, why "awake"
surgery might become more common.
Regional anesthesia is less expensive than general
anesthesia, there are fewer complications
and side effects, and faster recovery times. And, of
course, general anesthesia is always
available if patients change their minds. See
"Going
Under the Knife, with Eyes and Ears Wide Open" by Jan
Hoffman, New York Times, 03/26/2017)..
Since the 19th century, modern "scientific" medicine has generally disdained purely "empirical" treatments that are known to be efficacious, even though their scientific bases are not known. Nevertheless, general anesthesia has been universally adopted despite the fact that its underlying mechanisms remain a matter of considerable mystery.
Based on our understanding
of the molecular and cellular bases of neural activity, it
seems plausible that general anesthetics could temporarily
and reversibly disrupt neural activity in one of several
ways:
To complicate things further, the various classes of anesthetic agents appear to have somewhat different mechanisms of action. For example, many intravenous "hypnotic" drugs -- including propofol, barbiturates such as thiopental, and benzodiazepines such as diazepam -- appear to interact with gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter, to increase the time that chloride ion channels are open, resulting in a hyperpolarization of cell membranes. However, ketamine, another intravenous anesthetic, interacts with excitatory N-methyl-D-aspartate (NMDA) receptors instead. Natural and synthetic opioid anesthetics such as fentanyl, of course, act on opioid receptors, inhibiting presynaptic release of neurotransmitters such as acetylcholine and substance P. However, even in high doses these drugs do not, by themselves, induce loss of consciousness. For this purpose, they are often combined with nitrous oxide and oxygen. Nitrous oxide, for its part, has effects on NMDA receptors similar to those of ketamine. Current evidence is broadly consistent with anesthetic action on both synaptic excitation and inhibition, with the contribution of each process varying from agent to agent.
The molecular and cellular mechanisms by which inhaled anesthetics such as isoflurane achieve their effects have been subject of intense investigation and debate. According to the Myer-Overton rule known since the late 19th century, there is a strong correlation between the potency of an anesthetic gas and its solubility in lipids. One early suggestion was that the expansion of nerve cell membranes effectively closed the ion channels by which sodium enters the cell to induce an action potential.
However, It is now believed that the inhalants bind directly to specific pockets of relevant proteins rather than altering the lipid bilayer itself. In this way, they might create a dynamic block of the "lock and key" channels involved in synaptic excitation; some anesthetics also intensify synaptic inhibition. Although the general view is that anesthetics act on the postsynaptic side, there are some indications that they inhibit presynaptic neurotransmitter release as well.
The concept of balanced anesthesia implies that there are likely to be a number of separate mechanisms working together to produce analgesia (lack of pain), a sleep-like loss of consciousness (sometimes referred to as "hypnosis"), immobility (voluntary responses to surgical stimuli, as opposed to the spinal reflexes suppressed by muscle relaxants such as vecuronium), and amnesia (lack of memory for surgical events). According to one proposal, inhalants such as isoflurane, which induce both immobility and amnesia, achieve these effects by different routes: immobility by acting on GABA receptors in the spinal cord, and amnesia by suppressing activity in the hippocampus.
As it happens, the specific proteins affected by inhaled anesthetics are receptors for GABA, among other neurotransmitters. Thus, the inhaled anesthetics may share a mechanism with the intravenous anesthetics after all. Along the same lines, the inhaled anesthetics share some pharmacological properties, such as tolerance, withdrawal, and cross-tolerance, with alcohol and sedative hypnotics such as barbiturates; this suggests that there may be a common mechanism uniting the inhaled and the intravenous anesthetics as well. On the other hand, there are now a number of anesthetic agents that violate the Meyer-Overton rule, and it is known some gases can bind to the proteins implicated in anesthesia yet not cause anesthesia. Although much attention has focused on GABA, Hans Flohr has implicated NMDA instead. Both nitrous oxide and ketamine act as antagonists on NMDA receptors, blocking glutamate, an excitatory neurotransmitter -- as does xenon, a newly developed anesthetic. Even if the intravenous anesthetics share a final common pathway with some inhaled anesthetics, other inhalants may achieve the same effects by rather different means.
These considerations
suggest a "dual-process" theory, in which general
anesthesia occurs by virtue of one or another of two
general processes:
 Some
theorists have sought to solve the mystery of
anesthesia by invoking another mystery, namely quantum
theory. Roger Penrose, a British mathematical
physicist, and Stuart Hameroff, an American
anesthesiologist, have famously speculated that
consciousness is a product of certain processes
described by quantum theory (Penrose, 1989, 1995;
Penrose & Hameroff, 2011; Hameroff, 2013).
Some
theorists have sought to solve the mystery of
anesthesia by invoking another mystery, namely quantum
theory. Roger Penrose, a British mathematical
physicist, and Stuart Hameroff, an American
anesthesiologist, have famously speculated that
consciousness is a product of certain processes
described by quantum theory (Penrose, 1989, 1995;
Penrose & Hameroff, 2011; Hameroff, 2013).
Briefly:
Anyway, within the
context of the quantum theory, Hameroff has
proposed that these processes take place in
microtubules -- proteins found in the walls of
neurons that are shaped like hollow tubes.
Although the conventional view is that
microtubules serve a structural function,
supporting the structure of the cell, it is also
true that they are built out of proteins -- and
certain proteins are known to be the site of
anesthetic activity. Penrose and Hameroff contend
that consciousness is actually a product of
processes occurring in this microtubular
cytoskeleton, which are in turn magnified by the
neuron itself.
The Penrose-Hameroff theory of both consciousness and anesthesia has attracted a great deal of interest, and something like it has been endorsed by Eccles, but at this stage it remains highly speculative, and has been criticized on both logical and empirical grounds.
The quantum theory of consciousness has been criticized as excessively speculative, but its status might actually be worse than that -- an instance of what the Nobel physics laureate Murray Gell-Mann has called "quantum flapdoodle". The basic problem is that there is no reason to think that the "micro" (really, subatomic) world of quantum mechanics has anything to do with the "macro" world of classical physics -- that is, the real world in which human experience, thought, and action actually take place. For example, in the Unconscious Quantum (1995), Victor Stenger calculated that quantum mechanics operates only when a system's mass (m), speed (v), and distance (d) are on the order of Planck's constant (h). Because the properties of neurotransmitters exceed this limit, Stenger argues that quantum mechanics cannot provide a useful description of what is going on in the nervous system.
Or, as I like to
put it, whether the strings of string theory
vibrate in 10 or 11 or 26 dimensions, apples
still fall, planets still revolve around their
suns, the universe still expands -- and people
still think and behave.
Roger Penrose,
Nobel Laureate
|
Clinically, the
success of general anesthesia is marked by three
criteria:
Evaluated in
these terms, anesthesia is almost always
successful, with far fewer than 1% of surgical
patients report any awareness during
surgery.
In general surgery, intraoperative awareness and postoperative recall are usually attributable to light anesthesia, machine malfunction, errors of anesthetic technique, and increased anesthetic requirements -- for example, on the part of patients who are obese or abuse alcohol or drugs. The incidence of surgical recall arises in special circumstances, such as trauma, cardiac, or obstetrical surgery, where cardiovascular circumstances dictate lighter planes of anesthesia. Even then, the incidence of surgical recall is remarkably low -- in part because even in the absence of anesthesia, the benzodiazepines often used for sedation are themselves amnestic agents.
In fact, modern anesthetic practice may underestimate the incidence of intraoperative awareness by interfering with postoperative memory. That is to say, an inadequately anesthetized patient may be aware of surgical events at the time they occur, but be unable to remember them later because of sedative-induced anterograde amnesia.
However low, the possibility of surgical awareness means that, in addition to monitoring various aspects of vital function during the operation, the anesthetist must also monitor the patient's state of consciousness, or anesthetic depth. This task would be made easier if psychology and cognitive science could reach consensus on the neural or behavioral correlates of consciousness. In the absence of such criteria, anesthesiologists have often been forced to improvise.
One set of standards simply relies on measures of anesthetic potency. Research has determined the minimum alveolar concentration (MAC) of inhalant which prevents movement in response to surgical stimulation in 50% of patients; MAC-aware is the concentration required to eliminate awareness of the stimulation. As a rule, MAC-aware is roughly half of MAC, suggesting that some of the movement in response to surgical stimulation is mediated by subcortical structures, and does not necessarily reflect conscious awareness. Similar standards for adequate anesthesia, based on blood plasma levels, have been worked out for intravenous drugs such as propofol.
It should be noted that the operational definition of MAC-Aware means that 50% of patients will be aware of surgical events despite the presence of anesthetic -- although a dose amounting to about 1.3 MAC does seem to do the trick.
Nevertheless, it is important to supplement knowledge of dose-response levels with more direct evaluations of the patient's conscious awareness. Unfortunately, many obvious clinical signs of consciousness -- such as talking or muscle movement in response to surgical stimulation are obviated by the use of muscle relaxants.
 To make things worse,
the use of muscle relaxants in balanced
anesthesia makes it possible to perform
surgery under lighter doses of anesthetic
agents -- increasing the risk of
intraoperative awareness and postoperative
recall at the same time as they decrease the
risk of anesthetic morbidity. In fact, it
was recognized early on that the use of muscle
relaxants increased the risks further, by
preventing inadequately anesthetized patients
from communicating their intraoperative
awareness to the surgical team -- a situation
reminiscent of Harlan Ellison's
science-fiction classic, I Have No Mouth
and I Must Scream (1967).
To make things worse,
the use of muscle relaxants in balanced
anesthesia makes it possible to perform
surgery under lighter doses of anesthetic
agents -- increasing the risk of
intraoperative awareness and postoperative
recall at the same time as they decrease the
risk of anesthetic morbidity. In fact, it
was recognized early on that the use of muscle
relaxants increased the risks further, by
preventing inadequately anesthetized patients
from communicating their intraoperative
awareness to the surgical team -- a situation
reminiscent of Harlan Ellison's
science-fiction classic, I Have No Mouth
and I Must Scream (1967).
Of course, the simple fact that anesthesia impairs conscious recall does not mean that anesthetized patients lack on-line awareness of what is going on around them. In principle, at least, they could experience an anterograde amnesia for surgical events similar to that which occurs in conscious sedation. Or, perhaps, a retrograde amnesia. In either case, the possibility remains open that the patient is aware during surgery, but forgets it completely thereafter.
In the absence of a reliable and valid physiological index of conscious awareness -- something that is not likely to be available any time soon -- what is needed is some kind of direct behavioral measure of awareness, such as the patient's self-report. In balanced anesthesia, of course, such reports are precluded by the use of muscle relaxants.
But a variant on balanced anesthesia known as the isolated forearm technique (IFT), developed by Tunstall (1977), actually permits surgical patients to directly report their level of awareness in response to commands and queries. Because muscle relaxants tend to bind relatively quickly to receptors in the skeletal musculature, if the flow of blood is temporarily restricted to one forearm by means of a tourniquet, the muscles in that part of the body will not be paralyzed. And therefore, the patient can respond to the anesthetist's instruction to squeeze his or her hand, or raise their fingers -- that is, if they are aware of the command in the first place.
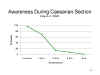 Interestingly, response
to the IFT is not highly correlated with
ostensible clinical signs of consciousness.
Nor does it predict postoperative recollection
of intraoperative events. In one study (King
et al., 1993), more than 40% of patients
receiving general anesthesia for caesarian
section responded positively to commands; yet
only about 2% had even fragmentary
recollections of the procedure. On the
assumption that a patient who responds
discriminatively to verbal commands is clearly
conscious to some extent, the IFT indicates
that intraoperative awareness is somewhat
greater than has previously been believed. On
the other hand, discriminative behavior also
occurs in the absence of perceptual awareness,
as in cases of "subliminal" perception, masked
priming, and blindsight. Estimates of
intraoperative awareness may indeed be
suppressed by an anterograde amnesia, which
effectively prevents patients from
remembering, and thus reporting, any awareness
that they experienced during surgery.
Interestingly, response
to the IFT is not highly correlated with
ostensible clinical signs of consciousness.
Nor does it predict postoperative recollection
of intraoperative events. In one study (King
et al., 1993), more than 40% of patients
receiving general anesthesia for caesarian
section responded positively to commands; yet
only about 2% had even fragmentary
recollections of the procedure. On the
assumption that a patient who responds
discriminatively to verbal commands is clearly
conscious to some extent, the IFT indicates
that intraoperative awareness is somewhat
greater than has previously been believed. On
the other hand, discriminative behavior also
occurs in the absence of perceptual awareness,
as in cases of "subliminal" perception, masked
priming, and blindsight. Estimates of
intraoperative awareness may indeed be
suppressed by an anterograde amnesia, which
effectively prevents patients from
remembering, and thus reporting, any awareness
that they experienced during surgery.
The IFT is a useful tool for the anesthesiologist, but there are other, less direct, ways of monitoring surgical awareness that are more popular.
Traditionally,
some anesthesiologists have relied on presumed
autonomic signs of conscious pain and stress,
such as the PRST score based on four
factors:
In modern practice, most methods for monitoring the depth of anesthesia involve the central nervous system.
 One common monitoring
technique employs event-related potentials
(ERPs, also known as evoked potentials, or
EPs) elicited in the EEG by weak
somatosensory, auditory, or even visual
stimulation. The ERP, which is obtained by
averaging the brain's response to repeated
stimulation, consists of three components:
One common monitoring
technique employs event-related potentials
(ERPs, also known as evoked potentials, or
EPs) elicited in the EEG by weak
somatosensory, auditory, or even visual
stimulation. The ERP, which is obtained by
averaging the brain's response to repeated
stimulation, consists of three components:
Adequate anesthesia reduces the amplitude of the various peaks and troughs in the ERP, as well as the latency of various components representing brainstem response and early and late cortical responses. Of course, the late "cognitive" components of the ERP would be expected to disappear entirely during adequate anesthesia. An AEP index of consciousness reflects the degree to which the late "cognitive" components of the ERP are suppressed, and the three "mid-latency" components of are delayed with respect to their normal occurrence between 20 and 45 milliseconds after the stimulus.
Another EEG index of
consciousness is based on the EEG
power spectrum, derived by a fast
Fourier transform (don't ask) of the raw
EEG signal. To make a long story
short, the EEG can be broken up into four
basic bands based on
frequency.
Another derivative
of the raw EEG is provided by
bispectral analysis, a proprietary
algorithm (meaning that it is a patented
trade secret!) which employs a
complicated set of transformations to
yield a bispectral index (BIS)
based on a number of features of the
EEG, such as the amount of
high-frequency activation (indicating
wakefulness) and periods of "flat line"
EEG (indicating the lack thereof).
BIS
ranges from close to 100 in subjects who
are normally awake, to values well under
60 in patients who are adequately
anesthetized, and is clearly correlated
with brain-imaging measures of cortical
activity.
Although most physiological indices of anesthetic depth have been validated against such criteria as movement in response to painful surgical stimulation, they have also been compared to various aspects of memory performance. In one study, a 0.2% end-tidal concentration (a measure related to MAC) of isoflurane produced a substantial impairment of performance on a continuous recognition test even over retention intervals as short as 8 seconds, while a 0.4% end-tidal concentration reduced recognition after 32 seconds to zero. Another study showed similar effects for low and high doses of propofol. In a study comparing midazolam, isoflurane, alfentanyl, and propofol, a 50% reduction in recall was associated with an average BIS score of 86, while an average BIS of 64 yielded reductions of 95%.
Another
proprietary device making use of processed
EEG yields "stages" of
anesthesia, analogous to sleep
stages, ranging from A (fully awake)
to F (a absence of brain activity).
In
2010, McSleepy hooked up with
DaVinci, a surgical robot (where
the surgeon operates a set of
joysticks, but the actual cutting
is done by a machine), to perform
the first intercontinental surgery
-- a prostatectomy. The
patient was in Italy, but the
anesthesia was monitored and
delivered by McSleepy, and the
surgery itself was done by
DaVinci, all controlled from
McGill.
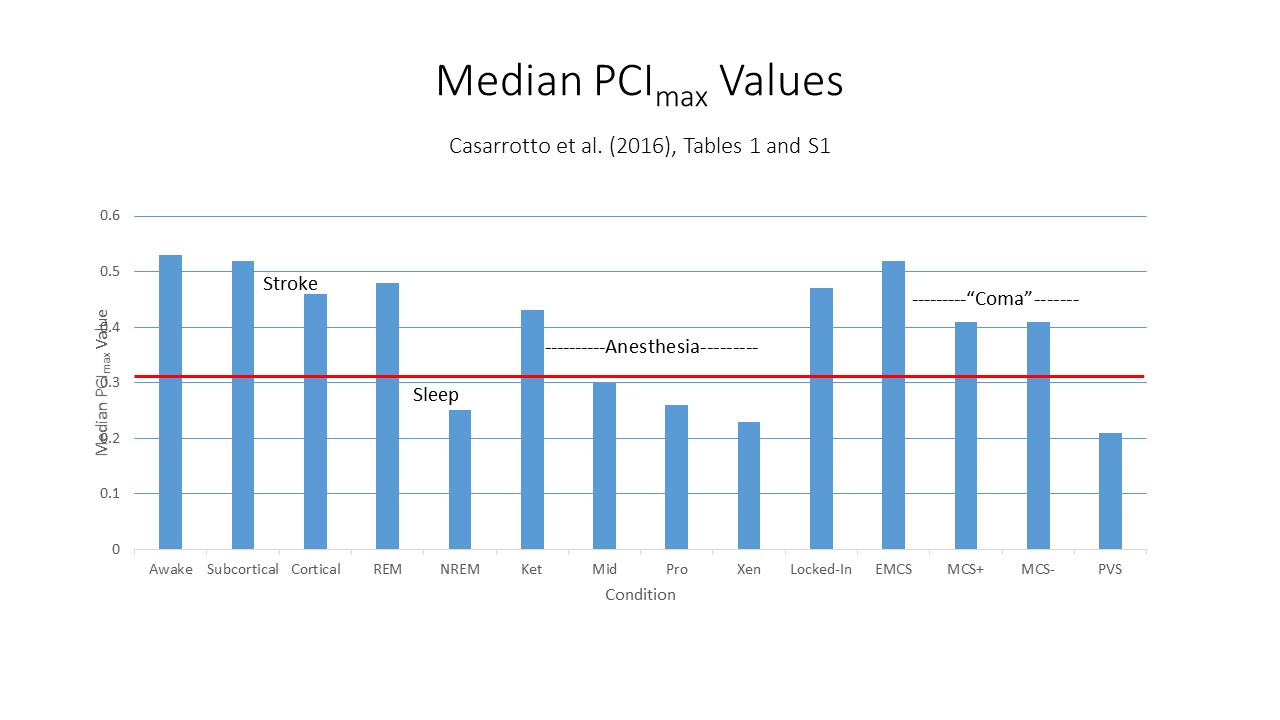 Another
approach to monitoring
anesthesia is
suggested by the
relies on the PCI
index of consciousness
discussed in the lectures
on Mind and Body.
Recall that Casarotto
et al. (2016)
performed a
"benchmarking" study
which established a
value of PCI* = .31
for distinguishing
between subjects who
are conscious and
those who are
not. This study
included four groups
of health subjects who
underwent general
anesthesia with
midazolam, propofol,
and xenon. All
three groups had
median PCImax
scores below the PCI*
threshold value of
.31. The
subjects who received
ketamine anesthesia
reported after
recovery from
anesthesia, that they
were aware of events
while the anesthesia
was in effect: they
showed PCImax
scores during
anesthesia that were
above the threshold
PCI* value of
.31. No such
report were given by
any of the subjects in
the other three
anesthesia
groups. This
suggests that PCI
scores would be useful
in monitoring depth of
general
anesthesia.
Another
approach to monitoring
anesthesia is
suggested by the
relies on the PCI
index of consciousness
discussed in the lectures
on Mind and Body.
Recall that Casarotto
et al. (2016)
performed a
"benchmarking" study
which established a
value of PCI* = .31
for distinguishing
between subjects who
are conscious and
those who are
not. This study
included four groups
of health subjects who
underwent general
anesthesia with
midazolam, propofol,
and xenon. All
three groups had
median PCImax
scores below the PCI*
threshold value of
.31. The
subjects who received
ketamine anesthesia
reported after
recovery from
anesthesia, that they
were aware of events
while the anesthesia
was in effect: they
showed PCImax
scores during
anesthesia that were
above the threshold
PCI* value of
.31. No such
report were given by
any of the subjects in
the other three
anesthesia
groups. This
suggests that PCI
scores would be useful
in monitoring depth of
general
anesthesia.
A note is in order about the side-effects of general anesthesia. There is some evidence that general anesthesia can lead to post-operative delirium (POD), including disorientation, hallucinations, and problems with "short-term" memory similar to those seen in the amnesic syndrome. POD generally dissipates pretty quickly. More concerning are occurrences of postoperative cognitive dysfunction (POCD), which lasts much longer and includes a wider range of problems in attention, memory, learning, and thinking. The deeper the anesthesia, as measured by BIS or similar indices, the greater the risk. Older patients are especially at risk for both POD and POCD. There is apparently less risk to infants and children, possibly because the immature brain is more plastic than the mature, adult brain. But the risks at any age have to be balanced against the fact that most modern surgeries wouldn't be possible at all without general anesthesia, and those that would be possible would also be pretty unpleasant (ask any Civil War veteran amputee). For more details, see "Hidden Dangers of Going Under" by Carina Storrs, Scientific American, 04/2014; and "The Risks of Going Under" by Andrea Anderson, Scientific American Mind, 03-04/2017).
While adequate general anesthesia abolishes conscious recollection of surgical events by definition, it is possible that unconscious (or, for that matter, conscious) intraoperative perception may lead to unconscious postoperative memory that influences the patient's subsequent experience, thought, and action outside of phenomenal awareness.
In fact, clinical lore within anesthesiology includes the "fat lady syndrome", in which an overweight patient's postoperative dislike of her surgeon is traced to unkind remarks he made about her body while she was anesthetized. Nevertheless, documented cases are hard to find.
In the late 1950s and early 1960s David Cheek, a Los Angeles physician and hypnotherapist, described a number of patients who, when hypnotized, remembered meaningful sounds that occurred in the operating room -- particularly negative remarks. Cheek claimed to have corroborated these reports, and attributed unexpectedly poor postoperative outcomes to unconscious memories of untoward surgical events. Unfortunately, the interview method he employed, hypnotic "ideomotor signaling", is highly susceptible to experimenter bias, and information that would corroborate such memories is not always available. Accordingly, the possibility cannot be excluded that patients' postoperative "memories", recovered through this technique, are confabulations.
Despite these methodological problems, Cheek's suggestion was subsequently supported by Bernard Levinson, who as an experiment staged a bogus crisis during surgery. After the anesthesia had been established (with ether), the anesthesiologist, following a script, asked the surgeon to stop because the patient's lips were turning blue. After announcing that he was going to give oxygen, and making appropriate sounds around the respirator, he informed the surgeon that he could carry on as before. One month later, Levinson hypnotized each of the patients -- all of whom had been selected for high hypnotizability and ability to experience hypnotic age regression -- and took them back to the time of their operation. Levinson reported that four of the ten patients had verbatim memory for the incident, while another four became agitated and anxious; the remaining two patients seemed reluctant to relive the experience. Levinson's provocative experiment suggested that surgical events could be perceived by at least some anesthetized patients, and preserved in memory -- even if the memories were ordinarily unconscious, and accessible only under hypnosis.
Despite Levinson's report, unconscious perception during general anesthesia remained largely unexplored territory until the matter was revived by Henry Bennett. Inspired by the apparent success of Cheek's "ideomotor signaling" technique for revealing unconscious memories, Bennett gave anesthetized surgical patients a tape-recorded suggestion that, when interviewed postoperatively, they would perform a specific behavioral response, such as lifting their index finger or pulling on their ears. Although no patient reported any conscious recollection of the suggestion, approximately 80% of the patients responded appropriately to the experimenter's cue. Bennett, following Cheek, suggested that unconscious memories were more likely to be revealed with nonverbal than with verbal responses.
 At about the
same time, Evans and Richardson
reported that intraoperative
suggestions, delivered during
general anesthesia, led to improved
patient outcome on a number of
variables, including a significantly
shorter postoperative hospital stay.
Again, the patients had no conscious
recollection of receiving these
suggestions. Although this study was
not concerned with memory per se,
the apparent effects of suggestions
on post-surgical recovery certainly
implied that the suggestions
themselves had been processed, if
unconsciously, at the time they
occurred.
At about the
same time, Evans and Richardson
reported that intraoperative
suggestions, delivered during
general anesthesia, led to improved
patient outcome on a number of
variables, including a significantly
shorter postoperative hospital stay.
Again, the patients had no conscious
recollection of receiving these
suggestions. Although this study was
not concerned with memory per se,
the apparent effects of suggestions
on post-surgical recovery certainly
implied that the suggestions
themselves had been processed, if
unconsciously, at the time they
occurred.
As it happens, subsequent studies have failed to confirm the findings of either Bennett et al. or Evans and Richardson. And more recently, a double-blind study inspired by Levinson's report, in which non-patient volunteers received sub-anesthetic concentrations of either desflurane or propofol, failed to obtain any evidence of memory for a staged crisis. Nevertheless, these pioneering studies, combined with an increasing interest in consciousness and unconscious processing within the wider field of psychology and cognitive science stimulated a revival of interest in questions of awareness, perception, and memory during and after surgical anesthesia, which have been carried out with progressively improved paradigms.
Of particular importance to this revival was the articulation, in the 1980s, of the distinction between two different expressions of episodic memory -- explicit and implicit. To review: In one of
the first controlled studies of
implicit memory following
surgical anesthesia, Kihlstrom
et al. worked with patients
receiving isoflurane anesthesia
for elective surgery.
Through earphones, these
patients were played an auditory
list of 15 paired associates
consisting of a familiar word as
the cue and its closest semantic
associate as the target -- e.g,
ocean-water. The stimulus
tape was presented continuously
from the first incision to the
last stitch, for an average of
67 repetitions over an average
of 50 minutes. In the recovery
room, the patients were read the
cue terms from the stimulus
list, as well as a closely
matched set of cues from a
control list of paired
associates, and asked to recall
the word with which each cue had
been paired on the list read
during surgery: this constituted
the test of explicit memory. For
the test of implicit memory,
they were read the same cues
again, and asked simply to
respond with the first word that
came to mind. The subjects
recalled no more target words
from the presented list than
from a control list, thus
showing that they had very poor
explicit memory for the
experience. On the
free-association test, however,
they were more likely to produce
the targeted response from the
presented list, compared to
control targets, thus displaying
a priming effect. Compared to
explicit memory, which was
grossly impaired (as would be
expected with adequate
anesthesia), implicit memory was
relatively spared.
In one of
the first controlled studies of
implicit memory following
surgical anesthesia, Kihlstrom
et al. worked with patients
receiving isoflurane anesthesia
for elective surgery.
Through earphones, these
patients were played an auditory
list of 15 paired associates
consisting of a familiar word as
the cue and its closest semantic
associate as the target -- e.g,
ocean-water. The stimulus
tape was presented continuously
from the first incision to the
last stitch, for an average of
67 repetitions over an average
of 50 minutes. In the recovery
room, the patients were read the
cue terms from the stimulus
list, as well as a closely
matched set of cues from a
control list of paired
associates, and asked to recall
the word with which each cue had
been paired on the list read
during surgery: this constituted
the test of explicit memory. For
the test of implicit memory,
they were read the same cues
again, and asked simply to
respond with the first word that
came to mind. The subjects
recalled no more target words
from the presented list than
from a control list, thus
showing that they had very poor
explicit memory for the
experience. On the
free-association test, however,
they were more likely to produce
the targeted response from the
presented list, compared to
control targets, thus displaying
a priming effect. Compared to
explicit memory, which was
grossly impaired (as would be
expected with adequate
anesthesia), implicit memory was
relatively spared.
Despite this early success, subsequent studies employing similar paradigms produced a mix of positive and negative results.
 For
example, Cork et al. precisely
replicated the procedure
employed by Kihlstrom et al.
with another group of patients
receiving sufentanyl, and found
that explicit and implicit
memory were equally impaired.
Although the two studies, taken
together, suggested the
interesting hypothesis that
different anesthetic agents
might have different effects on
implicit memory, a more
parsimonious conclusion might
have been that the isoflurane
effects were spurious.
For
example, Cork et al. precisely
replicated the procedure
employed by Kihlstrom et al.
with another group of patients
receiving sufentanyl, and found
that explicit and implicit
memory were equally impaired.
Although the two studies, taken
together, suggested the
interesting hypothesis that
different anesthetic agents
might have different effects on
implicit memory, a more
parsimonious conclusion might
have been that the isoflurane
effects were spurious.
In a debate at the Second International Symposium on Memory and Awareness in Anesthesia, held in 1992, experimental psychologists and anesthesiologists agreed that memory for events during anesthesia had not yet been convincingly demonstrated by an overwhelming body of research.
Over the
next few years, however, the
literature began to settle, so
that in 1996 a comprehensive
quantitative review by Merikle
and Daneman of 44 published
studies concluded that
adequately anesthetized patients
can, indeed, show postoperative
memory for unconsciously
processed intraoperative events.
 Although
the more recent literature
continues to contain a mix of
positive and negative results,
there are simply too many
positive findings, from too many
different implicit memory
paradigms, to be ignored. At the
same time, the literature
contains enough negative
studies, and other anomalous
results, to warrant further
investigation.
Although
the more recent literature
continues to contain a mix of
positive and negative results,
there are simply too many
positive findings, from too many
different implicit memory
paradigms, to be ignored. At the
same time, the literature
contains enough negative
studies, and other anomalous
results, to warrant further
investigation.
For example, in their 1996 review Merikle and Daneman concluded that the evidence for unconscious processing during general anesthesia was not limited to "indirect" measures of implicit memory, and extended to "direct" measures of explicit memory as well. This is a surprising statement, given that adequately anesthetized patients lack conscious recollection by definition. However, these authors included in their survey only the few tests of explicit memory that encouraged guessing, and excluded the many studies that discouraged guessing. While guessing yields a more exhaustive measure of conscious recollection, it is also true that guessing can be biased, unconsciously, by priming itself. Therefore, it is likely that some of the "explicit" memory identified by Merikle and Daneman is, in fact, contaminated by implicit memory. In support of this idea, a study employing the "process dissociation" procedure confirmed that postoperative memory was confined to automatic priming effects, and not conscious recollection.
A persisting issue is whether postoperative implicit memory might be an artifact of fluctuations in anesthetic depth which occur naturally during surgery. To some extent, this question was addressed in a new review of the literature, by Deeprose and Andrade (2006), which included 24 studies that employed formal (rather than clinical) assessments of anesthetic depth by means of the isolated forearm technique, auditory evoked potentials, or processed EEG (such as the Bispectral Index, spectral edge frequency, or Narcotrend). This review yielded mixed evidence generally favoring the hypothesis that perceptual priming was often spared during anesthesia. But no evidence that semantic priming was also preserved. There was more repetition priming observed in studies that employed a relatively light plane of anesthesia, compared to studies that employed deeper planes, but in all cases the anesthesia was clinically adequate, so there is no question that the preserved priming occurred only in patients who were in some sense "awake" during presentation.
In what is perhaps the best of these studies, Iselin-Chaves and her colleagues (2005, 2006). Instead of adopting the usual format of a comparison of explicit and implicit memory (e.g., comparing stem-cued recall with stem-completion), these investigators opted to use only a stem-completion test. However, they employed Jacob's Method of Opposition and Process-Dissociation Procedure to separate out the automatic (unconscious) and controlled (conscious) contributions to task-performance. In their experiment, 48 patients anesthetized with isoflurane or propofol (but without sedative premedication) were presented with a list of 40 words, each word repeated 40 consecutive times. There was also an unanesthetized control group.
Then,
within 36 hours of surgery, each
patient performed a
stem-completion test under
Inclusion and Exclusion
instructions. The patients
produced 17% of targets under
both conditions. That is,
they produced the same number of
targets when they were
instructed to exclude any they
consciously remembered, as they
did when there were instructed
to include those that they
consciously remembered. By
contrast, the controls produced
49% of the targets under the
Inclusion instructions, and only
15% of the targets under the
exclusion instructions.
Obviously, most of the patients'
stem-completion performance was
mediated by automatic priming,
while most of the controls'
performance was mediated by
conscious recollection.
During
surgery, depth of anesthesia was
monitored by the bispectral
index, and individual test items
were classified according to the
average BIS score obtained
during their presentation.
For the patients, conscious
recollection did not vary with
BIS score -- after all, even
"light" anesthesia is enough to
impair explicit memory.
But the automatic component,
representing unconscious
priming, was much larger than
the controlled component,
representing conscious
recollection.
This study
has been criticized for its
reliance on average BIS
scores, which leave open the
possibility that the spared
priming reflected conscious
processing occurring during
natural fluctuations of
anesthetic depth. In
response, Iselin-Chaves and her
colleagues (2006) re-analyzed
their data, classifying each
target in terms of the maximum
BIS score obtained during its
presentation. The results
were very much the same, except
-- not surprisingly -- less
priming was observed for items
presented under the vary deepest
levels of anesthesia.
Still, it has to be pointed out
that considerable priming
occurred for items presented
during "adequate" anesthesia,
and that "adequate" anesthesia
was sufficient to take the
conscious, controlled component
of task-performance almost to
zero. There was priming
for items presented during
anesthesia, and this priming was
spared even when explicit memory
was grossly impaired.
Most work on implicit memory employs tests of repetition priming, such as stem- or fragment-completion, in which the target item recapitulates, in whole or in part, the prime itself -- for example, when the word ashtray primes completion of the stem ash-. Repetition priming can be mediated by a perception-based representation of the prime, which holds information about the physical properties of the item, but not about its meaning. But there are other forms of priming, such as semantic priming, where the relationship between prime and target is based on "deeper" processing of the prime -- for example, when the prime cigarette primes completion of the stem ash- with -tray as opposed to -can. Semantic priming requires more than physical similarity between prime and target, and must be mediated by a meaning-based representation of the prime. The distinction between repetition and semantic priming is sometimes subtle. For example, in the isoflurane study described earlier, the paired associates presented as primes were linked by meaning, but because both elements of the pair were presented at the time of study, the priming effect observed could have been mediated by a perception-based representation, rather than a meaning-based one. The point is that implicit memory following surgical anesthesia is fairly well established when it comes to repetition priming, but conclusions about semantic priming are much less secure. Fewer studies have employed semantic priming paradigms, and relatively few of these studies have yielded unambiguously positive results. If semantic priming occurs at all following general anesthesia, it is most likely to occur for items presented at relatively light levels of anesthesia, as indicated by indices such as BIS. At deeper planes of anesthesia, implicit memory -- if it occurs at all -- is likely to be limited to repetition priming.
Priming effects are evidence of implicit memory, but they can also serve as evidence of implicit perception -- a term coined to refer to the effect of an event on experience, thought, and action, that is attributable to a stimulus event, in the absence of (or independent of) conscious perception of that event. Implicit perception is exemplified by "subliminal" perception of degraded stimuli, as well as neurological syndromes such as "blindsight" and neglect. In general anesthesia, the patients are presumably unaware of the priming events at the time they occurred. For that reason, evidence of implicit memory following general anesthesia is also evidence of implicit perception.
Link to the
website for the 8th
symposium on Memory and
Awareness in Anesthesia, to
be held in 2011 at the
Medical College of
Wisconsin, Milwaukee.
Link
to a
brief history of this
symposium (several of the
symposium proceedings have
been published).
The distinction between perception-based and meaning-based priming may have implications for the use of intraoperative suggestions to improve post-surgical outcome. As noted earlier, a positive report by Evans and Richardson helped stimulate this line of research to begin with. If subjects unconsciously retain information about surgical events, it might indeed be possible for them to benefit from therapeutic suggestions offered to them while they were anesthetized. On the other hand, if implicit memory following anesthesia is limited to repetition priming, implying that the anesthetized patient's state of consciousness does not permit semantic analysis of the intraoperative message, it is hard to see how such suggestions could have any effects at all.
In fact,
as noted earlier, attempts to
replicate the Evans and
Richardson study have been
largely unsuccessful, and the
Evans and Richardson study
itself has been criticized on a
number of grounds:
The suggestions
were evaluated
double-blind. As an
additional feature, all
patients received
patient-controlled
postoperative
analgesia. This
provided an objective
measure of the amount of
pain they experienced: if
the therapeutic suggestions
worked, patients who
received them would be
expected to request less
medication than those who
did not.
 As
As  it
it  happened, there
were no significant differences
between the three groups of
patients in terms of either
post-operative pain reports,
requests for morphine, or
nausea. In other words,
intraoperative therapeutic
suggestions had no more effect
on postoperative outcome than
did pre-operative
suggestions of the same sort --
or, for that matter, the pre-
and intraoperative reading of
short stories.
happened, there
were no significant differences
between the three groups of
patients in terms of either
post-operative pain reports,
requests for morphine, or
nausea. In other words,
intraoperative therapeutic
suggestions had no more effect
on postoperative outcome than
did pre-operative
suggestions of the same sort --
or, for that matter, the pre-
and intraoperative reading of
short stories.
Intraoperative suggestions will do no harm, and patients may derive some "placebo" benefit from the simple knowledge that they are receiving them during surgery. To the extent that intra-operative suggestions do some good, the limitations on information processing during anesthesia may mean that any positive effects are more likely to be mediated by their prosody, and other physical features, than by their meaning: a soothing voice may be more important that what the voice says. If anesthesiologists want patients to respond to the specific semantic content of therapeutic messages, such messages are probably better delivered while patients are awake, during the pre-operative visit that is already established as the standard of care.
General anesthesia is sometimes referred to as a controlled coma, and indeed anesthetized patients superficially resemble comatose patients:
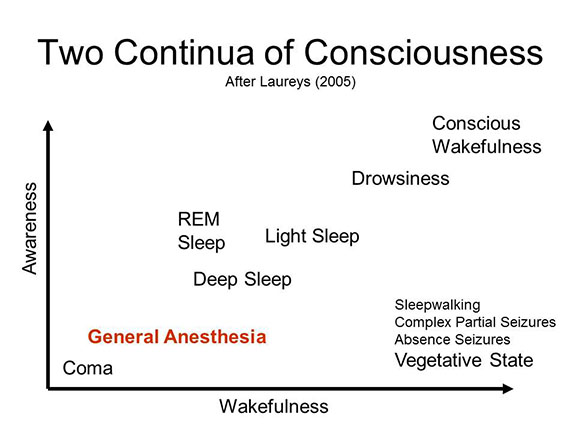 Like
coma, general anesthesia
underscores two basic
dimensions of
consciousness --
wakefulness and
awareness. Like
comatose patients,
adequately anesthetized
surgical patients seem
to lack both these
qualities.
Like
coma, general anesthesia
underscores two basic
dimensions of
consciousness --
wakefulness and
awareness. Like
comatose patients,
adequately anesthetized
surgical patients seem
to lack both these
qualities.
This page last revised 07/28/2023.