Psychosomatics
As interesting as the neural correlates of consciousness are, they represent only one side of the mind-body problem -- to wit, how does body affect (i.e., produce) mind? The other side is represented by the question of how the mind affects the body.
In philosophy, this is commonly discussed in terms of the problem of free will. We know (or we think we do) that our thoughts, feelings, and desires causes us to do what we do. But in psychology and psychiatry, this aspect of the mind-body problem is represented by the problem of psychosomatic interactions -- that is, physical diseases that are somehow caused by the patient's beliefs, attitudes, feelings, and other mental states.
In his Notes Upon a Case of
Obsessional Neurosis (also known as the case of the "Rat
Man", 1909/1953), for example, Sigmund Freud wrote of "the leap from a mental
process to a somatic innervation, which can never be fully
comprehensible to us". He
repeated the point in his Introductory Lectures on
Psycho-Analysis (1916-1917), referring to the "puzzling
leap" from the mind to the body.
The leap from the mind to the body is at least as mysterious as the leap from the body to the mind. So, another project for science is to find out how the brain does this -- how, precisely, beliefs and other conscious mental states affect the functioning of our bodies, as reflected in phenomena like placebo effects and psychosomatic interactions.
But first we have to discover whether, indeed, we need to take such things seriously. There is a medical literature which disputes the importance, and even the existence, of psychosomatic effects.
Moreover, like dualism itself,
psychosomatic effects have a bad reputation, being associated
with a kind of vulgar form of Freudian psychoanalysis in which
a cigar, for example, is never allowed just to be a
cigar. Consider the following formulations taken from Psychosomatic
Medicine, a classic psychoanalytic treatise by Franz
Alexander (1950):
Here, for example,
is Alexander's (1950) psychoanalytic formulation of the etiology
of peptic ulcer.
Ulcers are
perhaps the classic example of the psychosomatic connection
between stress and disease. A modern
psychosomatic formulation of ulcers would abandon the Freudian
mumbo-jumbo, and simply talk about the effects of stress.
For ulcers, at least in theory, the weakest link lies somewhere in the stomach. And there may be other psychosomatic illnesses -- or, at least, illnesses that have a psychosomatic component -- where the weakest link lies elsewhere in the gastrointestinal system. Irritable bowel syndrome (spastic colon), comes to mind, implicating the large intestine. But the body contains many other systems, and the proper functioning of their components may well be compromised by stress.
Perhaps the best documented effect of stress on the body, of course, is hypertension, or high blood pressure. Theodore Roosevelt, Woodrow Wilson, and Franklin Delano Roosevelt all developed hypertension while in office, and Bill Clinton (who, admittedly, also had a famous love of cheeseburgers) had heart surgery after leaving office. Famously (and controversially), Friedman and Rosenhan estimated that what Friedman called "Type A" behavior -- basically, leading a high-stress lifestyle -- increased risk for coronary heart disease by almost 100%.
More
anecdotal, perhaps, is the loss of hair color. An article
in the New York Times noted that President Barack
Obama's hair had grayed noticeably in just 44 days as president
("44 Days in the White House, and the Hair? Grayer
Already" by Helene Cooper, 03/05/2009). Actually, as the
article notes, his hair began to gray noticeably even before he
became President, perhaps a reflection of the stress of the
two-year long campaign for the Democratic nomination, and then
the presidency itself (the two photographs, taken from the Times
website, show the President in 2007, on the left, and in 2009,
on the right). Other presidents, including Bill Clinton
and George W. Bush, also grayed noticeably while in office (but
not Ronald Reagan, who was quite upfront about dyeing his
hair).
![]() Not
anecdotal at all, research by Elissa Eppel, a psychologist at
UCSF, has documented that exposure to chronic stress can shorten
the telomeres, "caps" on the ends of chromosomes that
serve to protect them during replication. Telomere length,
in turn, is a biological marker for aging, meaning that stress
actually hastens the biological aging process. (Image from
"The Science of Living Longer and Better" by Fran Smith, National
Geographic, 01/2023.)
Not
anecdotal at all, research by Elissa Eppel, a psychologist at
UCSF, has documented that exposure to chronic stress can shorten
the telomeres, "caps" on the ends of chromosomes that
serve to protect them during replication. Telomere length,
in turn, is a biological marker for aging, meaning that stress
actually hastens the biological aging process. (Image from
"The Science of Living Longer and Better" by Fran Smith, National
Geographic, 01/2023.)
Stress can cause, or at least exacerbate disease, and so it would make sense that stress reduction can be an important part of the healing process. And, in fact, there is considerable evidence that stress-reduction treatments, including biofeedback and various forms of meditation, can improve physical health. But there are limits to what stress-reduction can do. For example, a group of researchers famously reported that group psychotherapy led to an increase in survival for a group of women who had been treated for breast cancer. However, subsequent studies failed to confirm this finding, and the general consensus now is that the original finding was adventitious. Stress is bad for the body, and stress-reduction can help, the effects of stress and stress-reduction are likely to be at the margins, and psychological treatments for physical disease are probably best thought of as adjuncts, or complements, to standard medicine -- not as viable alternatives.
In fact, this modern psychosomatic formulation lies at the heart of the stress-disease connection studied by contemporary health psychologists. It appears that exposure to psychological stress, whether acute or chronic, increases a person's risk for a whole host of diseases, including mental illnesses such as depression, but also physical illness (Cohen et al., 2007).
We've known for a long time that the body's exposure to stress involves the secretion of adrenalin into the bloodstream, as part of the normal, reflexive "flight or fight" response. But one of the consequences of this is the subsequent release of another stress hormone, cortisol. Cortisol is normally a good thing, because it reduces inflammation of bodily tissues, but when it is released chronically, as in prolonged -- really prolonged -- exposure to stress, it can have deleterious effects on bodily functioning.
Here are just
a few of the physical consequences of the
prolonged release of cortisol:
Current psychobiological work on the stress-disease connection focuses on two neuroendocrine interactions between the nervous system and the endocrine system (Cohen et al., 2007): the hypothalamic-pituitary-adrenocortical axis (or HPA) and the sympathetic-adrenal-medullary axis (or SAM).
The
hypothalamic-pituitary-adrenocortical axis begins with
the hypothalamus, a subcortical structure, which releases a
substance known as the corticotrophin-releasing factor,
or CRF. CRF, in turn, stimulates the pituitary
gland to release the adrenocorticotropic hormone, or ACTH.
ACTH stimulates the adrenal glands to secrete cortisol,
which has a wide variety of effects on anti-inflammatory
processes, the metabolism of carbohydrates, fats, and
proteins, and glucogenesis.
The
sympathetic-adrenal-medullary axis begins with
activation of the sympathetic nervous system, during which the
adrenal medulla releases the hormones adrenalin and
noradrenalin. These catecholamines have a
variety of systemic effects on the cardiovascular and
pulmonary, hepatic (kidneys), skeletal, and immune
systems.
These effects have stimulated the development of whole new branches of psychology devoted to the study of psychoendocrine and psychoimmune interactions (because these interactions are obviously mediated by the nervous system, and nobody wants to leave the neuroscientists out, these are sometimes called psychoneuroendocrine and psychoneuroimmune interactions, respectively.)
That's all on the somatic side of the
modern psychosomatic formulation. What about the
psychological side -- in particular, what do we mean by stress?
A psychological definition of stress is implied in Walter B. Cannon's (1915) description of the "flight or fight" response. For Cannon, and others who are biologically inclined, "stress" refers to any environmental stimulus that elicits the "flight or fight" response from an organism. But from a psychological point of view, the environment that matters is the perceived environment. Which means that "stress" needs to be defined subjectively, in terms of the individual's perception of the environment.
Shelley Taylor, a social psychologist at UCLA who specializes in health psychology and the stress-disease connection, noted that Cannon based his description of the "flight or fight" response exclusively on the behavior of male laboratory animals. Further, she noted that females tend to give quite a different pattern of responses, which she characterized as "tend and befriend". According to Taylor, the "choice" between "flight or fight" and "tend and befriend" is largely determined by levels of sex hormones such as testosterone and estrogen.
Actually, though, the specific term stress was initially imported from physics and introduced into the psychological lexicon by Hans Selye (1936, 1956), as any event that challenges the organism's current level of physiological or psychological adjustment. Selye further distinguished between the distress caused by affectively negative events and eustress caused by affectively positive events. His point being that getting married can be as stressful as getting divorced.
Cohen and his colleagues (1999) offered a purely psychological definition of stress as "the perception that environmental demands tax or exceed adaptive capacity". Note, in this definition, that stress is instigated by perception. Objectively, it doesn't matter whether demands tax capacity. All that matters is subjective perception.
At a theoretical level, psychosomatic effects might dramatically illustrate the causal efficacy of consciousness. At a clinical level, these psychosomatic effects might even be put to practical use. At the same time, there is some tendency among many biologically oriented psychiatrists and clinical psychologists to dismiss psychosomatic effects as mere folklore of a past age, beneath scientific contempt.
From the standard biomedical perspective "real" diseases have known biological causes, and the "real" causes of mental illness are biological (genetic, neurochemical) in nature. Even the websites of such established organizations as the National Institute of Mental Health (NIMH) and the National Alliance for Mental Illness (NAMI) vigorously assert that such syndromes as anxiety and depression are "real diseases" because we now think that we know something about their biological underpinnings -- as if mental illness was not "real" unless it had a neurobiological cause!
A good example of the controversy over psychosomatic medicine concerns ulcers. Traditionally, peptic ulcers, whether gastric or duodenal, were commonly attributed to stress, and thus counted as "psychosomatic" in nature. Nevertheless, among many psychotherapists the underlying belief persists that mental states can have effects on bodily processes.
However, the
discovery by Marshall and Warren (1984) that patients with
ulcers were infected by a particular bacterium, Helicobacter
pylori (H. pylori) led many physicians to
reconstrue ulcers as an infectious disease, discounting any
psychological causes. In their initial study,
Marshall and Warren examined samples from the stomachs of a
number of patients who had sought treatment for
gastrointestinal distress (presumed ulcers). H.
pylori was present in more than 80% of patients who
actually had ulcers, but only about 50% of patients who
received diagnoses of gastric inflammation (gastritis),
excessive bile, or who proved to have no disease at all.
Their conclusion was that ulcers had an infection
origin, in H. pylori. For this discovery,
Marshall and Warren received the Nobel Prize for Physiology
and Medicine in 2005.
Marshall and Warren's discovery lent
strong support to those in the medical community who sought to
deny the psychosomatic assumption that stress and other mental
states could be the cause of physical disease. In fact,
Steven Hyman, then a prominent biological psychiatrist at
Harvard Medical School (soon to become the Director of the
National Institute of Mental Health, and subsequently Provost
of Harvard University), went so far as to write an article on
the discovery entitled "Another One Bites the Dust" (1994) --
meaning that ulcers represented another case where a putative
psychological cause had been disproved in favor of something
biochemical in nature.
Now, there's no doubt that many mental illnesses, including schizophrenia and some forms of depression, have biochemical causes. But that does not mean that psychological factors don't play a role in them, or that psychological factors aren't important causal agents in other forms of mental illness -- or, more to the point of the present discussion, that psychological factors don't play a role in causing physical illness.
Under the
psychosomatic hypothesis, diseases such as ulcers classify as
mental illnesses because their presumed cause is -- well, mental.
But the fate of ulcers exemplified a trend in the medical
community (and, for that matter, among some psychologists) to
prefer somatogenic over psychogenic theories
of mental illness. For example, Ralph Gerard, a
prominent American physiologist, once declared that "There is
for every twisted thought a twisted molecule". More
recently, Thomas Insel ("Faulty Circuits", Scientific
American, 2010), Director of the National
Institute of Mental Health, predicted that neuroimaging would
eventually redefine mental illnesses as neurological
illnesses".
The biologization of mental
illness involves a number of aspects:
The discovery of H. pylori had implications beyond our understanding of ulcers, because it severely undermined the psychosomatic hypothesis in general. In fact, the whole category of "psychosomatic" or "psychophysiological" disorders disappeared from the psychiatric lexicon (or, at least, from later editions of the Diagnostic and Statistical Manual for Mental Disorders), to be replaced by a category of "Psychological Factors Contributing to Medical Condition". Nevertheless, it turns out that there is good reason to doubt a purely infectious origin for peptic ulcers, and every reason to think that stress plays a causal role in ulcers after all.
Note, first, that even in the original study of Marshall and Warren, the "normal" patients, who proved to have no ulcers (or any other disease) also had relatively high levels of H. pylori infection. This is actually more true even than it appears from the Marshall and Warren study. Marshall and Warren conducted what is known as a retrospective study of ulcers, which began with a number of patients who reported gastrointestinal problems, and then looked in their stomachs for evidence of H. pylori. It turns out that such retrospective analyses can exaggerate the role of various causal factors. A better estimate of the true strength of a causal relationship is provided by a prospective study which begins with a random sample of the population.
Just
such
a study was reported by Nomura et al. (1994), who looked for
evidence of H. pylori infection in a sample of the
population, and then diagnosed the patients as to whether they
had gastric ulcers, duodenal ulcers, or no ulcers. As in
the Marshall and Warren study, the vast majority of patients
with ulcers proved to be infected with H. pylori
-- approximately 90%. But the control subjects
also showed high levels of infection: roughly 80% of patients
who were free of the disease were infected with H. pylori.
Hyman has a point: "stress" is a hard concept to measure precisely -- especially if you count "positive" stressors like marriage as well as "negative" stressors like divorce. If you know someone has ulcers, it's all too easy to look back at his premorbid history and find some stressors, to which you can attribute the ulcer. What's needed is empirical evidence that stress can cause ulcers.
Ideally, you'd take two groups of subjects, subject one group to high levels of stress, and then conduct biopsies to determine whether they developed ulcers. Of course, nobody is going to do such a study -- at least not on humans. But precisely that kind of study has been done, in an animal model, by Bruce Overmier and his colleagues at the University of Minnesota (1997)
But how to
operationalize stress? As noted earlier,
physiologists, and many psychologists, prefer to define stress
as any event which challenges an organism's current level of
adaptation. A different approach is based on research by
a number of psychologists from the field of animal learning --
including Overmier, Martin E.P. Seligman, and Steven Maier,
who were the pioneers in this area (and who were all graduate
students together at the University of Pennsylvania; and Susan
Mineka and myself, who were in the next generation of graduate
students at Penn, and very much influenced by their
work. Together, Overmier, Seligman, and Maier discovered
learned helplessness, in which prior experience with
uncontrollable shock retards avoidance learning. Mineka
and Kihlstrom expanded this work to propose a new perspective
on experimental neurosis, in which laboratory animals
appeared to show "neurotic" behavior as a result of various
learning experiences. Mineka and Kihlstrom proposed that
experimental neurosis was induced by aversive events that had
one or both of two qualities:
In their experimental paradigm,
Overmier and Murison (Current Directions in Psychological
Science 1997, Behavioral Brain Research 2000)
and their colleagues employed lab-raised rats who are
presumably free of H. pylori infection -- or if they
are infected, random assignment of rats to the various
experimental conditions insures that the groups do not differ
in this respect.
The
basic
finding of their research is that prior exposure to
unpredictable and/or uncontrollable shock increases the effect
of RIW on ulceration. In one study, pretreatment with
shock that was both unpredictable (P-) and uncontrollable (C-)
increased ulceration, over what was observed following RIW
alone; but less ulceration occurred when the
pretreatment was unpredictable (P-) but controllable (C+).
In another study predictable (P+) but uncontrollable (C-) shock
also increased ulceration, over RIW alone.
Apparently, controllability is more important than predictability -- when the shock is controllable, ulceration is decreased. Because controllability is more important than predictability, Overmier and Murison label this the helplessness pretreatment.
Other
studies
confirmed the causal role of stress in gastric
ulceration. Overmier and Murison have studied an animal
model (rats) of peptic ulcers that shows a clear role for
psychological stress in triggering ulcers. Ulceration is
increased when the helplessness pretreatment is administered
in the same environmental context as the RIW treatment.
And ulceration was also increased when the rats received
"free" shocks during the rest period following the RIW
treatment -- the more so when the uncontrollable shocks are
also unpredictable.
So, it turns out that stress, in the form of the acute RIW treatment, especially when it is preceded by the (more chronic) helplessness pretreatment, causes ulcers after all.
 Extrapolating from
the Overmier and Murison research, and with due regard to the
discovery of H. pylori by Marshall and Warren, we can
offer a diathesis-stress model for the development of
ulcers. In medicine, including psychiatry, such models
postulate that an acute episode of some illness (whether cancer
or the common cold, schizophrenia or depression) is caused by
the interaction of two factors, diathesis and stress.
Extrapolating from
the Overmier and Murison research, and with due regard to the
discovery of H. pylori by Marshall and Warren, we can
offer a diathesis-stress model for the development of
ulcers. In medicine, including psychiatry, such models
postulate that an acute episode of some illness (whether cancer
or the common cold, schizophrenia or depression) is caused by
the interaction of two factors, diathesis and stress.
Applying this model to ulcers:
Placebo
effects have been called the "jewel in the crown" of
psychosomatic medicine, because they appear to show how
patients' beliefs about the treatment they are getting
influence the outcome of treatment. In the standard
definition (Shapiro & Shapiro, 1997),
In clinical trials, placebos are typically used as controls to reveal whether new pharmacological agents actually have any specific effects on medical outcomes. In order to be approved by the US Food and Drug Administration, new drugs must be shown to be safe and effective -- the latter usually by comparison of the active drug to an inert placebo.
But first things first: What's this about placebos being powerless after all. How can placebos be powerless, if the pharmaceutical industry has to take account of them?
Because
drug companies don't have to have such a group, there are
remarkably few studies in the medical literature that have a
no-treatment control group. Nevertheless, between their
original 2001 study and a 2004 follow-up, (Hrobjartsson and Gotszche were
able to identify 156 studies.
Now, the H&G study has been criticized on a number of grounds -- chiefly, their exclusion of laboratory (as opposed to clinical studies), and their overly broad definition of a "placebo" to include almost any pharmaceutically inert treatment, no matter how implausible. But still, the onus is now on placebo researcher to demonstrate that placebos really do have effects, and that they are powerful enough to be respected by health-science professions.
But beyond whatever advantage they can provide in the treatment of illness, placebos are of theoretical interest because of the light they can shed on the problems of mind and body. Usually, the mind-body problem is framed as unidirectional: how brain processes can produce conscious mental states. But placebos, and other psychosomatic effects, remind us that there is another mind-body problem: how mental states can affect bodily functioning. Documenting these effects, and understanding their underlying psychological and biological mechanisms, is the great challenge posed by placebos.
One area where placebo effects have been clearly demonstrated is in the area of pain.
For example, it turns out that
placebos have "pharmacological" properties (Evans,
1974).
Many consumers, and some physicians and drug companies, suspect that generic drugs, which cost less, are also less effective than their brand-name or reference-drug equivalents. And the Food and Drug Administration actually found that to be the case for Budeprion XL 300 mg, the generic equivalent of the brand-name Wellbutrin XL 300 mg. From a psychobiological point of view, this is puzzling, because by definition generic drugs are biologically equivalent to their brand-name reference drugs. All that is missing is the label. Where generics differ in effectiveness from their brand-name reference drugs, there may well be some as-yet unappreciated problem in manufacture. But it may also be the case that generic equivalents lack the "placebo power" of their brand-name equivalents, which carry both the cachet of a famous drug manufacturer and an extra cost.
 The role of belief in placebo effects is
dramatically illustrated by an analysis by Evans (1974, 1985)
of studies in which placebos were compared to a number of
different pharmacological agents in the treatment of
pain. Remarkably, Evans found that placebo efficiency --
the ratio of positive outcomes with placebo to positive
outcomes with drug -- was constant, at about .55, across a
wide variety of drugs. In other words, if patients
believed they were taking morphine, patients who really got
placebo got roughly half the pain relief as patients who
really got morphine; but if patients believed they were taking
aspirin, those who really got placebo got roughly half the
relief as patients who really got aspirin. Although
Evans did not perform the analysis, the implication of his
research is that patients who believe they are getting
morphine will get more pain relief than patients who believe
that they are getting aspirin, even though all are getting
placebo!
The role of belief in placebo effects is
dramatically illustrated by an analysis by Evans (1974, 1985)
of studies in which placebos were compared to a number of
different pharmacological agents in the treatment of
pain. Remarkably, Evans found that placebo efficiency --
the ratio of positive outcomes with placebo to positive
outcomes with drug -- was constant, at about .55, across a
wide variety of drugs. In other words, if patients
believed they were taking morphine, patients who really got
placebo got roughly half the pain relief as patients who
really got morphine; but if patients believed they were taking
aspirin, those who really got placebo got roughly half the
relief as patients who really got aspirin. Although
Evans did not perform the analysis, the implication of his
research is that patients who believe they are getting
morphine will get more pain relief than patients who believe
that they are getting aspirin, even though all are getting
placebo!
Another area where placebo effects have been found to be substantial is in the area of depression.
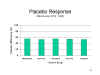
In a provocative paper entitled 'Listening
to Prozac and Hearing Placebo", Kirsch and Sapirstein (1998)
reviewed 28 published clinical trials of antidepressant
medications -- tricyclics and tetracyclics (e.g., Elavil and
Norval), selective serotonin reuptake inhibitors (e.g., Prozac),
other antidepressants, and other medications that were not
generally considered to be antidepressants, but which were being
tested "off label" for their antidepressant effects. Each
of these studies included a medication arm and a placebo
arm. But, in line with standard practice, none of them
included a no-treatment control group. For this purpose,
Kirsch and Sapirstein turned to the psychotherapy literature,
where the standard design includes a group of patients who get
psychotherapy and a group that gets no treatment at all (e.g.,
by being put on a waiting list). In each of these studies,
depression before and after treatment was measured by standard
self-report questionnaires such as the Hamilton Depression
Scale.
From their point of view, then, placebos are powerful indeed.
Kirsch and his colleagues (2002) made a
similar point in a second study, which reviewed all clinical
trials of SSRIs for depression, regardless of whether they had
been published (for this they used the Freedom of Information
Act to access the FDA database). Again, the placebo was
about 80% as effective as the drug to which it was compared --
regardless of whether that drug was Prozac, Paxil, Zoloft,
Effexor, Serzone, or Celexa). Unfortunately, this study
did not include a no-treatment control group, but Kirsch's point
is that there's little question that placebos are powerful in
the treatment of depression - -almost as powerful as our most
powerful drugs.
Link to a segment of 60 Minutes, interviewing Prof. Irving Kirsch and others on placebo effects in the drug treatment of depression, broadcast on CBS 02/19/2012.
Placebos have also been found useful in the
treatment of irritable bowel syndrome (IBS), which is
characterized by abdominal pain, cramping, bloating,
constipation, and diarrhea. However, there are no signs of
physical damage to the gastrointestinal system, such as
inflammation (which would lead to a diagnosis of inflammatory
bowel disease, or IBD) or bleeding polyps
(which might lead to a diagnosis of colon cancer). For
this reason, thee are no specific tests for IBS (as opposed to
IBD), and in fact IBS is only properly diagnosed when IBD, colon cancer, and similar diseases
have been ruled out (it's also what makes IBS a syndrome
instead of a disease). The lack of diagnostic
signs has led some psychiatrists to suggest that IBS
is a somatoform illness --
that is, a mental illness whose symptoms involve physical
complaints. This point is controversial, but the fact of
the matter is that the standard of care for IBS involves
primarily psychosocial treatments, such as stress and lifestyle
management, as well as prescriptions for antidepressants.
Although IBS patients may also be instructed to alter their diet
(mostly by drinking lots of prune juice!), few if any
interventions are actually directed toward the gastrointestinal
system.
In a recent series of studies,
Ted Kaptchuk and his colleagues at Harvard Medical School
have found that placebos lead to significant symptom relief in
IBS patients. The studies are a little unusual in that
they employ placebo acupuncture rather than placebo pills.
From my own perspective, I would have thought that pills would
be the obvious vehicle for delivery of placebos to IBS patients, simply because pills are
swallowed and pass through the gastrointestinal
system. But Kaptchuk runs a program
in complementary and alternative medicine at HMS, where
there's a great deal of interest in acupuncture. And
while some physicians suspect that acupuncture is just a
placebo itself, or at least mostly placebo, there
is also such a thing as placebo acupuncture --
that is, a procedure that looks like acupuncture but which lacks the ostensibly active
ingredient.
Kaptchuk
et al. (2008) randomly assigned
a large group of IBS patients to one of three conditions:(1) Limited Placebo, in which patients
received sham acupuncture but extremely limited psychosocial contact (2)
Augmented Placebo, in which the patients received a
considerable amount of face-to-face social support from the
practitioner; and (3) a waitlist control which received no
acupuncture and no practitioner-patient interaction.
After three weeks of "treatment", the augmented acupuncture
group showed significant improvement on all measures,
compared to the waitlist controls, with the limited
acupuncture group falling in-between. Some of these patients continued to receive sham
acupuncture for another 3 weeks, with essentially the same
result.
The remaining patients were shifted "true" acupuncture: the comparison of true vs. sham acupuncture yielded no significant effects (Lembo et al., 2009), which is consistent with the idea that acupuncture itself is a placebo treatment.
To
make things
really interesting, Kaptchuk and his colleagues
(2010) actually told the patients that they were giving
them a placebo -- and it worked. Patients given "sugar"
pills clearly labeled as placebos -- what is called an "open
label" placebo -- got significant relief of pain and other
symptoms, compared to a control group that got no pills at
all. But why would subjects respond to something that they
had been told was pharmacologically inert? It has to do
with the context in which the placebos were taken.
Kaptchuk told the patients that placebos worked by mobilizing
"mind-body self-healing processes". So, the patients
didn't believe that the placebo was just an ineffective treatment; instead,
they probably believed that placebos actually work
through a psychosomatic process. So, the belief affected
the functioning of the gastrointestinal system.
But it's one thing to believe you're being given
an active drug, and to have that belief affect your physiology;
it's another thing to believe you're being given a placebo, and
to have that belief affect your physiology. Maybe
the patients didn't believe that they were being given
placebo. After all, in the balanced placebo design, some
subjects who are told they're getting placebo get the active
agent instead. On the other hand, maybe it's the
instructions that come with the placebo that are critical.
After all, the physician doesn't just hand a patient a pill,
saying "This is a placebo, take it". Instead, in this
study (and others of a similar sort conducted by Kaptchuk and
his associates) the placebo is surrounded by an actively
therapeutic context. Patients are informed of advances in
mind-body medicine; they're encouraged to believe that placebos
mobilize mind-body interactions; and they're told that their
placebo has been "designed especially" for them and their
particular problem. What it means, exactly, to have a
placebo "designed especially" for a particular person and a
particular problem isn't clear. But I suppose that just
goes to emphasize the importance of the psychosocial
context. Social psychologists tell us that beliefs are
stronger when they're acquired in a highly persuasive context,
and placebos appear to be no exception.
Kaptchuk argues that placebo
effects aren't simply a matter of "mind over matter" -- that
placebos have real physiological consequences. Placebos
given for pain, for example, release endogenous opioids, cannabinoids, and dopamine (a
neurotransmitter important in the brain's "reward"
system). The usual explanation for
placebo effects involves some sort of conditioning
procedure. If delivering an active analgesic
(analogous to an unconditioned stimulus) triggers a
physiological response that leads to pain reduction (an
unconditioned response), then delivering
a placebo analgesic might act as a
conditioned stimulus for the
release of endogenous opiates as a conditioned
response. It's a good hypothesis, and probably
largely correct. However, it is undercut by
instances where placebos are effective even though
the patient has had no prior experience with the
active drug.
Setting aside the effects of placebos per se, an increasing body of literature suggests that verbal suggestion -- that is, the communication of a belief from one individual to another -- can have effects on objectively measured physiological outcomes.
A number of controlled experimental and clinical studies in the area of psychosomatic medicine have employed variants of the symptom-provocation method familiar in the diagnosis and treatment of allergies and asthma. In this technique, a patient is stimulated with a substance hypothesized to cause an allergic reaction; if the allergen actually induces an allergic reaction, the patient is then treated with another substance, hypothesized to prevent or reduce the reaction (this is known as symptom neutralization).
For a variety of reasons, mostly historical, a great deal of research on psychosomatic interactions has involved hypnotic suggestions. However, it turns out that suggestion, and the beliefs that suggestion engenders, is more important than hypnosis per se.
 Perhaps the
granddaddy of all such studies is a clinical report by Mason
(published in the British Medical Journal, 1952, 1955)
of a 16 year-old boy with congenital icthyosiform
erythrodermia of Broq. Commonly known as "fish
skin disease", this syndrome is a hereditary disorder
affecting the skin, which becomes discolored and blackened,
horny, inelastic, fissured, and peppered with vascular
protuberances. The disease was extremely unsightly, not
to mention distressing to the patient. Conventional
treatment, involving skin grafts from unaffected portions of
the body, failed: the new areas acquired the erythrodermia as
well. As a last resort, Mason hypnotized the patient,
and suggested that the lesions would go away. But -- and
this is a very big but -- Mason did it right.
First, he suggested that the skin would clear on the patient's
left arm. After 5 days, the left arm -- but the left arm
alone -- began to clear, and was completely clear after 10
days. Then Mason gave similar suggestions targeting the
right arm, and then the patient's legs, and trunk. The
progressive remission of the skin lesions, highly correlated
with the suggestions, was documented photographically, both
after initial treatment and at a 4-year followup. (Mason
also attempted hypnosis with other cases of icthyosis, with
varying degrees of success.)
Perhaps the
granddaddy of all such studies is a clinical report by Mason
(published in the British Medical Journal, 1952, 1955)
of a 16 year-old boy with congenital icthyosiform
erythrodermia of Broq. Commonly known as "fish
skin disease", this syndrome is a hereditary disorder
affecting the skin, which becomes discolored and blackened,
horny, inelastic, fissured, and peppered with vascular
protuberances. The disease was extremely unsightly, not
to mention distressing to the patient. Conventional
treatment, involving skin grafts from unaffected portions of
the body, failed: the new areas acquired the erythrodermia as
well. As a last resort, Mason hypnotized the patient,
and suggested that the lesions would go away. But -- and
this is a very big but -- Mason did it right.
First, he suggested that the skin would clear on the patient's
left arm. After 5 days, the left arm -- but the left arm
alone -- began to clear, and was completely clear after 10
days. Then Mason gave similar suggestions targeting the
right arm, and then the patient's legs, and trunk. The
progressive remission of the skin lesions, highly correlated
with the suggestions, was documented photographically, both
after initial treatment and at a 4-year followup. (Mason
also attempted hypnosis with other cases of icthyosis, with
varying degrees of success.)
 In another classic of the hypnosis
literature involved the Mantoux reaction, a
diagnostic skin test for tuberculosis (still in use). After a
subcutaneous injection of purified protein derivative
tuberculin, a physician will measure the size of the induration
-- a raised, hardened, red blister created by the injection. A
positive reaction is indicated by a induration of a particular
size.
In another classic of the hypnosis
literature involved the Mantoux reaction, a
diagnostic skin test for tuberculosis (still in use). After a
subcutaneous injection of purified protein derivative
tuberculin, a physician will measure the size of the induration
-- a raised, hardened, red blister created by the injection. A
positive reaction is indicated by a induration of a particular
size.
 Black (1963) studied
four Mantoux-positive patients, all of whom were known to be
highly hypnotizable, giving
them a suggestion that "You will no longer react to the
injection as you did before... no redness, no swelling, no heat,
no itching, no pain...". And, for each of the four patients,
that's just what happened. Compared to pre-suggestion
measurements, both the size of the swelling and the size of the
erythema (the reddened portion) decreased. However, a skin
biopsy showed that the underlying histology was unaffected by
the suggestion. The suggestion targeted the superficial, visible
Mantoux reaction, and that's all that changed. But still!
Black (1963) studied
four Mantoux-positive patients, all of whom were known to be
highly hypnotizable, giving
them a suggestion that "You will no longer react to the
injection as you did before... no redness, no swelling, no heat,
no itching, no pain...". And, for each of the four patients,
that's just what happened. Compared to pre-suggestion
measurements, both the size of the swelling and the size of the
erythema (the reddened portion) decreased. However, a skin
biopsy showed that the underlying histology was unaffected by
the suggestion. The suggestion targeted the superficial, visible
Mantoux reaction, and that's all that changed. But still!
Mason employed a similar
approach in treating difficult cases of allergic reaction.
 In a classic study, two Japanese
investigators, Ikemi and Nakagawa (1962) employed a variant on the
symptom-provocation method to study the effects of suggestion on a
form of contact dermatitis (similar to poison ivy or poison oak)
induced by contact between a person's skin and the leaves of the
lacquer and wax trees common in Japan and other parts of East
Asia.
In a classic study, two Japanese
investigators, Ikemi and Nakagawa (1962) employed a variant on the
symptom-provocation method to study the effects of suggestion on a
form of contact dermatitis (similar to poison ivy or poison oak)
induced by contact between a person's skin and the leaves of the
lacquer and wax trees common in Japan and other parts of East
Asia.
 Based on a survey, 13 male high-school
students known to be sensitive to the leaves were recruited
for the study. After they were blindfolded, their arms
were brushed by the lacquer-tree or wax-tree leaves (depending
on their sensitivity), and were given the suggestion that the
plant was actually harmless: 11 of the 13 subjects showed a
reduced skin reaction to the poisonous leaves. In
another condition, they were brushed by the chestnut-tree
leaves, but told they were the leaves of the lacquer or wax
tree (depending on their sensitivity): all 13 subjects showed
signs of dermatitis.
Based on a survey, 13 male high-school
students known to be sensitive to the leaves were recruited
for the study. After they were blindfolded, their arms
were brushed by the lacquer-tree or wax-tree leaves (depending
on their sensitivity), and were given the suggestion that the
plant was actually harmless: 11 of the 13 subjects showed a
reduced skin reaction to the poisonous leaves. In
another condition, they were brushed by the chestnut-tree
leaves, but told they were the leaves of the lacquer or wax
tree (depending on their sensitivity): all 13 subjects showed
signs of dermatitis.
Sometimes, the suggestions were given while the subjects were hypnotized, but not on all instances. Accordingly, hypnosis had nothing to do with the outcome. The controlling factor was the subjects' beliefs about what they were touching -- beliefs influenced by the experimenters' suggestion, but beliefs nonetheless. Beliefs that had physiological consequences.
Link to the study by Ikemi and Nakagawa (1962).
Similarly, there is a large
clinical literature on the effects of hypnotic suggestion on
dermatological warts.
 Although
the Johnson and Barber study seemed to indicate that hypnosis
was a crucial variable, Spanos reasoned that hypnotic
suggestions might have worked better simply because, by virtue
of the myths and urban legends surrounding hypnosis, the
hypnotic suggestions were more believable. Accordingly,
Spanos, Stenstrom, & Johnson (1988) employed three groups
of subjects. One received typical hypnotic suggestions
for wart control. A second group received treatment from
a plausible "cold laser" machine, that was actually a
placebo. A third group received no treatment at
all. At 6-week followup, the subjects who had received
the hypnotic suggestions showed the greatest remission of
warts.
Although
the Johnson and Barber study seemed to indicate that hypnosis
was a crucial variable, Spanos reasoned that hypnotic
suggestions might have worked better simply because, by virtue
of the myths and urban legends surrounding hypnosis, the
hypnotic suggestions were more believable. Accordingly,
Spanos, Stenstrom, & Johnson (1988) employed three groups
of subjects. One received typical hypnotic suggestions
for wart control. A second group received treatment from
a plausible "cold laser" machine, that was actually a
placebo. A third group received no treatment at
all. At 6-week followup, the subjects who had received
the hypnotic suggestions showed the greatest remission of
warts.
 In a second study, Spanos et al. (1988) compared
four groups: hypnotic suggestion, nonhypnotic suggestion,
relaxation without suggestion, and no treatment. The
hypnotic and nonhypnotic conditions produced comparable
results, leading Spanos et al. to conclude that the imagery
contained in the suggestions, rather than hypnosis itself, was
the major factor. In both experiments, similar studies
have shown that both hypnotic and nonhypnotic suggestions can
lead to the remission of warts.
In a second study, Spanos et al. (1988) compared
four groups: hypnotic suggestion, nonhypnotic suggestion,
relaxation without suggestion, and no treatment. The
hypnotic and nonhypnotic conditions produced comparable
results, leading Spanos et al. to conclude that the imagery
contained in the suggestions, rather than hypnosis itself, was
the major factor. In both experiments, similar studies
have shown that both hypnotic and nonhypnotic suggestions can
lead to the remission of warts.
Although much research remains
to be done, it is fairly clear that hypnotic suggestion can
facilitate the treatment of burns.
This is a term given to episodes of sexual climax, male or
female, that occur in the absence of physical stimulation of
the penis, vagina, or clitoris. Long considered a myth,
or an urban legend, there is now some evidence that people can
think or imagine a sexual encounter that
results in an actual physiological orgasm.
The roots of this idea lie in research by Barry Komisaruk and
his colleagues (2004), who studied orgasm produced by tactile
self-stimulation in paraplegic women -- that is, women who
have suffered a complete break in the spinal cord at the level
of the 10th thoracic spinal nerve (T10) or above -- that is,
disconnecting the brain from the sensory nerves that supply
the pudendal, pelvic, and hypogastric regions of the
body. While that's interesting, it's not particularly
surprising: erection and ejaculation in men are spinal
reflexes which are preserved in paraplegia, provided that the
peripheral nerves themselves have not been damaged.
There's no reason why the same shouldn't be true for
women. What was really interesting is that the women
involved reported that they could feel the orgasm --
which isn't supposed to happen, given that the break in the
spinal cord. Based on fMRI evidence, Komisaruk has
suggested that these sensations are mediated by the Vagus
nerve (Cranial Nerve X), which has both afferent and efferent
components, and is spared in paraplegia.
Here's where the story gets interesting, because Komisaruk
and his colleagues also obtained evidence that women (these
subjects had intact spinal cords) could achieve full-fledged
orgasms simply by engaging in erotic thoughts and imagery,
without benefit of self-stimulation. Again, partly, this
isn't surprising. It is well known that men can achieve
erection simply by viewing erotic images, or reading or
listening to erotic narratives; similarly, women exposed to
erotic materials also show increased blood flow to the vagina,
which is the female cognate of male erection. What's
new, and surprising (at least to these researchers), is that
women (more than half of those tested) can have complete
orgasms merely by thinking erotic thoughts. This claim
does not rely on self-report, because the physiological
signature of orgasm is clearly apparent: by increases in blood
pressure, heart rate, and tolerance for pain; moreover, fMRI
shows that the so-called "pleasure centers" in the brain are
activated during orgasms brought on by imagination, and those
brought on by tactile stimulation. Moreover, women who
imagined tactile stimulation of their breasts and genitals
showed activation in the corresponding areas of somatosensory
cortex.
Of course, these orgasms aren't exactly spontaneous
-- it's not like they come unbidden, out of nowhere.
They're produced by thought, and memory, and
imagination. As such, they're yet another, if rather
dramatic, example of the effect of the mind on portions of the
body that lie outside the nervous system.
The fact that hypnosis is (probably) irrelevant to the psychosomatic effects of hypnotic suggestion has motivated some investigators to focus on suggestion alone, without any of the excess baggage associated with hypnosis.
Luparello and his associates
(1968, 1970) studied the effects of suggestion (nonhypnotic)
on airway reactivity in asthmatic patients. Asthma is
produced by constriction of the airway, as measured by the
Ga/TGV ratio. Low Ga/TGV ratios induce a bronchospasm,
or asthmatic reaction, which can be corrected by inhaling a
neutralizer.
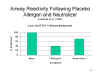 In one study, Luparello
and his associates (1968) administered a placebo allergen,
which reduced Ga/TGV ratios toward bronchospasm levels,
followed by a placebo neutralizer, which returned Ga/TGV
toward baseline.
In one study, Luparello
and his associates (1968) administered a placebo allergen,
which reduced Ga/TGV ratios toward bronchospasm levels,
followed by a placebo neutralizer, which returned Ga/TGV
toward baseline.
 In a more thorough
study, Luparello and his associates (1970) provided
patients with actual broncho-dilators or -constrictors,
accompanied by suggestions that the device contained either
a dilator or constrictor. When the patients were given
an actual dilator their airways dilated, as expected; but
there was less dilation when they were told that the dilator
was a constrictor. Similarly, when the patients were
given an actual constrictor, their airways constricted, as
expected; but there was less constriction when they were
told that the constrictor was a dilator.
In a more thorough
study, Luparello and his associates (1970) provided
patients with actual broncho-dilators or -constrictors,
accompanied by suggestions that the device contained either
a dilator or constrictor. When the patients were given
an actual dilator their airways dilated, as expected; but
there was less dilation when they were told that the dilator
was a constrictor. Similarly, when the patients were
given an actual constrictor, their airways constricted, as
expected; but there was less constriction when they were
told that the constrictor was a dilator.
The Luparello
studies support the earlier findings of Ikemi and Nakagawa,
and show that patients' beliefs can influence their bodies'
physical reaction to allergenic substances.
Challenge StudiesThe experiments
of Ikemi & Nakagawa and Luparello et al. fall into
an interesting category of medical research called a challenge
study, most famously used in the testing of new
vaccines. If you've got an infectious disease, and
a vaccine that you think will prevent it, one way to
test the vaccine is to give it to a bunch of people (and
a placebo to a control group), and then see how many
people in the vaccine group actually come down with the
disease. Sometimes the placebo arm is omitted, and
the vaccine group is simply compared to a group of
people who didn't get any treatment at all. But
this kind of clinical trial takes time, and usually
requires testing of very large numbers of subjects
(imagine, for example, that you're trying to detect the
effect of a vaccine on a disease which affects only
about 1% of those who have been exposed to it). A quicker way
to test a vaccine is to give it to a smaller group of
subjects and deliberately exposing them to the disease
-- the exposure is the challenge (of course, there has
to be a placebo or untreated control group as
well). The challenge method is very efficient, but
it is also highly controversial, because it appears to
violate the Hippocratic Oath to "first, do no
harm". Medical ethics generally prohibits
deliberately exposing people to a disease. But, as
I say, its been done -- mostly when the disease itself
is relatively benign (inconvenient, like allergy, rather
than deadly, like polio), or when a rescue treatment
(like an inhaler) is readily available. Challenge
trials were used most famously by Edward Jenner in his
work on the development of a smallpox vaccine (Jenner
coined the very word "vaccine" in 1796). They've
also been used in the development of vaccines for
typhoid, cholera, and malaria, among other
diseases.
|
Recently a new paradigm for the study of psychosomatic interactions has been introduced by Benedetti and his colleagues (2003). Inspired by both the placebo paradigm and the symptom-provocation paradigm, they compare two conditions, in both of which the patients get a treatment for their condition which is known to be effective. Thus, no placebos of any kind are involved. Instead, patients in the "open" condition are told that they are getting the treatment, while patients in the "hidden" condition receive the same treatment, only unbeknownst to them.
In
a study of diazepam treatment of postoperative
anxiety, patients who were told that they were getting
the drug reported less anxiety two hours later than those who
were not told; and when the administration was interrupted,
patients who were informed of this fact reported an increase
in anxiety, whereas those who were ignorant did not.
In
a study of morphine for postoperative pain,
patients who were told that they were getting the drug
reported less pain, compared to baseline, than those who were
not; and when the administration was interrupted, subjects who
were informed reported a greater increase in pain than those
who were not.
In
a study of subthalamic electrical stimulation for Parkinson's
disease, patients showed greater changes in movement
velocity when they were told the stimulation had begun, and
when they were told it had been interrupted.
Another provocative example
of psychosomatic interaction is presented by Viagra
(Sildenafil ciltrate), a popular pharmaceutical treatment for
male erectile dysfunction (commonly known as impotence).
Men who take Viagra are able to achieve and maintain erection
of the penis when they were previously unable to do so.
Viagra is generally considered to be a biological intervention
for impotence, and in fact its pharmacological action is well
known:
Still, further research may be
needed on whether sexual arousal enhanced by Viagra can be
produced with only visual (or, at least, non-tactile) "sexual
stimulation".
Among the many claims for psychosomatic
interactions, perhaps the most provocative is the idea of Ellen
Langer, a social psychologist at Harvard, that psychosocial
interventions can slow, or even
reverse, the aging process -- that "turning the clock back"
psychologically can turn the clock back physically as
well.
In a groundbreaking study, Langer and Rodin (1975) assigned a group of elderly nursing-home residents to take care of a potted plant, and also gave them a greater degree of choice in their daily schedules. A control group was given no choices; they were also given a potted plant, but told that the nursing-home staff would take care of it for them. On a follow-up 18 months later, twice as many residents in the experimental group were still alive, compared to the control group. This outcome suggested to Langer that, in fact, psychosocial factors -- like having choice and responsibility -- could, indeed, have palpable effects on bodily states.
In a later experiment, Langer and her colleagues (1990) took this idea to even farther extremes. In 1981, a group of eight elderly men, all in their 70s, was recruited to live for five days in lodgings that had been systematically modified to resemble a typical environment in 1959 -- right down to the music played over the "radio", the programs on the "TV", and the magazines on the coffee table. In the dining room and lounge, they discussed topics that were current in 1959 as if they were just happening -- and always in the present tense. And they wore clothes in the style of the late 1950s. For the entire time, the men were treated as if they were 20-something years younger, and they were instructed to really live as they had lived then -- not just to enact a role, but to inhabit it (like a Method actor). Langer et al. reported that, as a result, the men actually became "younger" on a variety of physical measures, compared to a control group who lived in the same space but without the special decorations and instructions. The experiment served as the basis for The Young Ones, a reality series initially broadcast by the BBC in 2010.
Eight men, five days, it's a
low-power experiment, but it supported Langer's belief that
one's mindset could have palpable
effects on physical health.
As discussed in later lectures on Attention and
Automaticity, Langer was also the earliest social psychologist to draw attention to the
automaticity of much social behavior -- she actually called it
"mindlessness", and she now explores the benefits of the opposite
mindset, which she calls mindfulness -- not exactly
the mindfulness associated with
certain forms of Eastern-style meditation,
as discussed in the lectures on Meditation, but simply active sentience -- taking note of changes in yourself and
the surrounding environment, avoiding familiar
categories, and other habits of
mind.
And she's also become a vigorous proponents of placebos in medicine. In one experiment, Crum and Langer (2007) worked with a group of hotel housekeepers. One group was (falsely) informed that their work, cleaning rooms and hallways, was actually vigorous physical exercise; a control group performed the same physical duties, but were given no information (or misinformation). They found that the maids in the experimental group actually lost weight, and showed improvements on other health measures as well. Their interpretation was that believing that they were engaging in physical exercise produced the effects of actual physical exercise. Of course, such studies have to be done carefully. It might be, for example, that the maids in the experimental group, once reminded about the benefits of exercise, actually increased their exercise levels -- for example, by walking up and down service stairways instead of taking the elevator.
It's
one thing for a placebo to relieve the
non-insubstantial psychological component of pain.
It's another thing entirely for hypnotic
suggestion to reduce
dermatological warts. Langer's
research -- including an
ongoing study testing whether a
"counterclockwise" manipulation can reverse
advanced cases of cancer -- is best viewed as an attempt to push
the boundaries of mind-body medicine to its
utmost limits.
As noted earlier, the placebo is the "jewel in the crown" of psychosomatic medicine. Unfortunately, most placebo research is on pain, and because pain is so subjective, placebo effects on pain might well be counted as instances of mental-mental causation -- that is to say, where a belief (that one has taken a drug) causes another belief (that one is not in pain).
This is also the case with respect to antidepressant medication. The placebo effects documented by Kirsch and his colleagues count as instances of mental-mental causation, where a belief (that one has taken a drug) causes another belief (that one is not in pain).
However, an emerging body of research suggests that placebos and other psychological interventions can have effects on objective, physiological outcomes as well. As always, further research is required.
Medicine commonly distinguishes between disease, defined as pathological anatomy or physiology, and illness, or the subjective experience of disease. If placebos affect only illness, helping patients to feel better, that may be enough. But if placebos affect disease as well, helping patients actually get better, that is even better, especially for those who are interested in the mind-body problem (Kihlstrom, 2008).
These considerations suggest
that there are two, maybe three, quite different kinds of
psychosomatic effects, which have to be distinguished.
It is not surprising -- at least, not to a psychologist -- that belief, expectation, and suggestion can have effects on the person's own mental state. And it's not surprising -- not to a dualist or a materialist, anyway -- that beliefs, expectations, and suggestions can have effects on the state of the person's central nervous system -- given that mental states are produced by the brain to begin with. The most provocative, perhaps the most convincing, and probably the most revolutionary evidence for psychosomatic interactions will be found in the body outside the central nervous system. such evidence would be incontrovertible evidence for psychosomatic effects.
That there are such effects is assumed by most proponents of behavioral (or psychological) medicine, who take an interest in the connection between stress and disease, leading to the development of whole new fields like psychoneuroendocrinology and psychoneuroimmunology, which search for the biological mechanisms by which the mind effects the body.
More work needs to be done, obviously, but taken together, studies of stress and disease, placebo effects, and the physiological effects of suggestion and other forms of social influence indicate that there is still plenty of life left in the psychosomatic hypothesis that mind can affect the body. In the 1950s, the Soviet psychologist Platonov published a book on psychosomatic medicine entitled The Word as a Physiological and Therapeutic Factor (1955). Given the importance of words in representing our thoughts, ideas, experiences, and beliefs, Platonov's work may yet prove prophetic. By showing how mental states can exert effects on bodily processes, this literature offers a new perspective on mind-body relations. Mind is not just a product of the body. Body is also a product of the mind.
Studies of the neural correlates of consciousness suggest that we can't get away from self-reports of phenomenal experience. And studies of placebos and psychosomatics suggest that mental states influence bodily processes. It appears that mind matters after all!
For an interesting and illustrated!) discussion of psychosomatic and placebo effects, with particular attention to "spiritual healing", see "Mind Over Matter" by Erik Vance, National Geographic, 12/2016). The basic question addressed in the article is: "How does a belief become so potent it can heal?".
In the psychosomatic syndromes, the patient's mental state affects objectively observable changes in anatomy and/or physiology outside the nervous system -- causing ulcers, acne, dysmenorhea, and the like. In some respects, the opposite side of the coin is represented by embodiment -- the idea that mental processes can be shaped by bodily states, the sensorimotor context in which they occur. The general idea behind embodiment is that cognition occurs in a widely distributed system that includes the body and the environment as well as the head.
Embodied
cognition has been formally defined by Glenberg et al.
(2013) as follows: thinking is grounded in
action. This viewpoint is reminiscent of Bruner's
famous adage, and here I am paraphrasing, that "The purpose of
perception is action"). These actions are performed by
bodies in environments. Thinking (by
which Glenberg means al cognition) is
not divorced from the body, but is strongly influenced by
both the body and the environment.
Recall from the lectures on The Mind-Body Problem that UCB philosopher Alva Noe has expressed similar ideas about consciousness itself. While most philosophers would simply say that consciousness is a product of brain processes, Noe believes that brains are necessary, but not sufficient, for consciousness. Consciousness also requires a body, which is in communication with the brain, and an environment to be conscious of.
Goldinger (2016), a colleague of Glenberg's at Arizona State
University (who is actually a critic of embodied cognition),
has summarized embodiment
in terms of six principles.
- Many cognitive psychologists think that knowledge is represented in the mind amodally, as abstract symbols -- perhaps like the 0s and 1s in a computer, rather than as modality-specific images.
- Actually, most cognitive psychologists acknowledge that there are both abstract "meaning-based" knowledge representations, and concrete "percption-based" ones, such as visual and auditory images.
- The strong version of embodied cognition denies that there are any abstract, amodal knowledge representations at all. Instead knowledge is embodied in sensory experience and motor action. Our knowledge of the world consists in what Gibson would call its affordances for action.
- The weak version of embodied cognition allows for abstract knowledge representations, but argues that embodied knowledge goes beyond mental imagery, and is a lot more important that cognitive psychologists think it is.
Embodied
cognition is also sometimes called grounded cognition.
Larry Barsalou, a leading figure in the embodied
cognition movement, is among those theorists who actually
denies that knowledge is represented symbolically.
Instead, he argues that cognition is grounded in
perception, action, and experience. He argues that
simulation is important for all aspects of cognition, and that
retrieving and using knowledge entails a re-enactment
of the experiential states that accompanied knowledge acquisition. Among the examples he cites:
Similarly, in Mind in Motion (2019),
Barbara Tversky (widow of Amos Tversky, in case you were
wondering) has argued that our status as animals -- that is,
animate beings -- who act by moving around in a physical world,
lies at the core of our cognitive abilities. Like other
proponents of embodiment, she challenges the notion that mind is
an abstract entity independent of the body. Human minds
can't be duplicated by silicon chips, much less beer cans linked
together by string (as a famous argument for Strong AI
imagined). She notices, for example, the number of
"motion" metaphors for thinking: "arrange and rearrange,
enlarge, stretch, join, copy, add, scramble, subtract, lift,
glue, push, fold, mix, toss, embellish, separate, nail, scatter,
bury, eliminate, turn, elevate, and poke holes in both real
objects and mental ones". These metaphors for thought, all
involving motion in and through space, give her hook its
title. Like some other theorists of embodiment, she
points out that, at least since the invention of writing,
and even more so now in the age of the internet and Google,
minds aren't the only things that perform cognitive work.
Much of it is offloaded into the physical world.
The program for embodied cognition has been worked out most thoroughly in the domain of perception -- which is quite reasonable, considering that perception is so closely tied both to sensory experience and action (remember the Brunerian aphorism: "The purpose of perception is action").
To demonstrate what research on
embodied perception looks like, consider a program of research
on slant perception by Dennis Proffitt and his
colleagues at the University of Virginia. Slant is one of
the basic problems in perception, along with the perception of
size, distance, motion, and figure-ground relations. For
example, perception of slant is important if you're going to
walk up a hill or climb a set of stairs. In his
experiments, Proffitt asks subjects to estimate the slope of an
actual hill located on the (very hilly) UVA campus.
By way of comparison:
Anyway, Proffitt asked his subjects to make their estimates in three different ways.
When subjects make verbal
estimates of slant, they overestimate wildly. Maybe it's
because they have an inaccurate sense of angles, but that can't
be the whole story, because their visual estimates, which don't
require them to state an angle in degrees, are also
inaccurate. But haptic estimates are very accurate indeed.
Subjects
who are (relatively) fatigued
from jogging also grossly overestimate the slope of a hill, as
do subjects who are carrying a heavy backpack. But not if
they make their estimates haptically instead of verbally or
visually.
Proffitt's
explanation is that the verbal and visual tasks reflect the
subject's explicit, conscious perception, "in which hills look
steeper than they are" -- a kind of visual illusion. By
contrast, the haptic task is very accurate, because it is
closely tied to the body's mechanisms for visually guided
action, and not susceptible to the illusions that affect
(infect?) conscious visual perception. conscious
overestimation is actually adaptive. Consider the kinds of
hills we encounter in everyday life, like 1º-9º. We can
manage these, but the difference between, say a 5 slope and a 6
slope is actually quite significant for locomotion. In
psychophysical terms, that's where overestimation tends to
occur, and that's where overestimation tends to occur. If
we overestimate the slope of a 6º grade, we'll be motivated to
try to find an easier climbing route -- especially if we're
tired or overweight. So overestimation is good for planning
action. But this same overestimation is not good for
actually executing action. Consider: even if we
think that a 5º grade is actually 10º, when we go to climb it we
don't actually lift our feet twice as high! No, because
the perception that guides action is embodied, we lift our feet
just the right amount -- no matter how tired or heavy we
feel. Visually guided action, as opposed to
visually informed planning, is closely linked to the
body and the environment.
Another area where
embodiment plays an important theoretical role is emotion (e.g.,
Niedenthal, 2007). Mainstream cognitive psychology tends
to think of emotion as an abstract "tag" added to the amodal,
symbolic representation of some concept or experience --
"Weddings are happy occasions", "Dissections are disgusting",
etc. (e.g., Bower, 1980). In contrast, theories of
embodied emotion argue that emotions are grounded in, and
represented by modality-specific sensory, motor, and
interoceptive activity. In a manner reminiscent of
the James-Lange theory of emotion, these patterns of
physiological activation, when consciously perceived, are
the emotion. And when emotions are remembered, or thought
about, or perceived in other people, these same patterns of
physiological activity are reinstated, so that the emotional
state itself is re-experienced. More to the point, in the
context of mind-body relations, when these emotion-specific
bodily states are reinstated, the emotion itself is reinstated
as well, and then spills over to affect cognitive processing --
shaping perception, memory, and thought.
Here are some examples from Niedenthal's work (disclosure: Paula worked as an undergraduate research assistant in my laboratory at the University of Wisconsin, where she was also strongly influenced by the perceptual-motor theory of emotion espoused by Howard Leventhal). Recall Paul Ekman's idea that certain basic emotions such as happiness, sadness, anger, and fear) are expressed as specific patterns of activity in the facial musculature. Niedenthal and others have discovered that forming these facial expressions, even in neutral stimulus situations, leads subjects to actually experience the corresponding emotions -- and for those emotional states to affect perception, memory, and judgment.
So, in these ways
certain bodily states generate particular mental -- in this
case, emotional states, even in the absence of relevant
stimuli. Again, this happens because emotions are not
represented abstractly and symbolically. Rather, emotions
are embodied. Niedenthal writes (2007, p. 1003):
In theories of embodied cognition, using knowledge -- as in recalling memories, drawing inferences, and making plans -- is thus called "embodied" because an admittedly incomplete but cognitively useful reexperience is produced in the originally implicated sensory-motor systems, as if the individual were there in the very situation, the very emotional state, or with the very object of thought. The embodiment of anger might involve tension in muscles used to strike, the enervation of certain facial muscles to form a scowl, and even the rise in diastolic blood pressure and in peripheral resistance, for example. The concept of reenactment and related concepts such as simulation, resonance, and emulation are widely accepted in theories of embodied cognition, but many different mechanistic neural accounts of it have been proposed. One promising possibility is that simulation is supported by specialized "mirror neurons" or even an entire "mirror neuron system," which maps the correspondences between the observed and performed actions.
Theories of embodiment are all the rage now in some quarters, but they aren't without their critics.
For
example, Mahon (2015; Mahon & Caramazza, 2008) has argued
conceptual processing -- even thinking about concrete concepts,
such as hammer and running is unimpaired in
neurological patients with sensory-motor deficits. If so,
then retrieving and using conceptual knowledge doesn't require
any kind of embodied re-enactment. All that is required is
abstract, amodal, symbolic representations of conceptual
knowledge concerning characteristic features,
subordinate-superordinate relationships, and the like.
And, for that matter, there are other neurological patients with
category-specific deficits in conceptual processing -- in
classifying objects as animals, for example -- who have
no sensory-motor impairments (Mahon & Caramazza,
2009). Therefore, the brain ystems for conceptual
processing and for sensory-motor processing must be
distinct. Or, put another way, conceptual processing is
disembodied after all.
More
generally, Stephen Goldinger et al. (2016) -- Goldinger is
actually a colleague of Glenberg's at ASU! -- has proposed that,
however much the notion of embodiment might inform our
understanding of perception and emotion, it is simply irrelevant
to a wide variety of topics in cognitive psychology, from
attention (the cocktail party phenomenon and Stroop
interference) through memory (the serial-position effect and the
post-event misinformation effect) to language (the
word-superiority effect and phoneme restoration effect) to
thinking (insight problem-solving and the availability
heuristic).
Goldinger et al. conclude that "The emperor has a body, but no clothes" -- but this seems unfair. There is clearly a case to be made for embodiment in aspects of perception that are closely linked to action, and also for emotion. But the strong view of embodied cognition, in which cognition is driven entirely by sensory, motor, and affective processes, is clearly wrong. There are two many counterexamples. But a weaker view is certainly viable:
This page was last updated 07/07/2020.