General anesthesia is sometimes described as a "controlled
coma", in which the anesthesiologist induces a temporary loss
of consciousness on the part of the patient, and then restores
it again after the surgery is over. But what about
uncontrolled coma -- the sometimes permanent loss of
consciousness that occurs in cases of severe brain
injury?
Preface: Defining Altered States of Consciousness
The principal problem in developing a scientific approach to consciousness is simply this: How can we make an objective study of subjective mental states? How can we gain public access to something that is essentially private?
We confront a similar problem when we turn to the topic of "altered" or "special" states of consciousness, where subjects report that their state of consciousness differs markedly, in at least some respects, from "normal". How can we study altered states of consciousness objectively? Well, by exactly the same means.
In a paper whose publication
marked the beginnings of the "consciousness revolution" in
cognitive psychology and cognitive science, Johann Stoyva and Joe
Kamiya (1966) proposed that converging operations be used
to identify and study various altered states of consciousness
(ASCs). An ASC was not identified with any one of these, but
the "diagnosis" of an ASC could be made with increasing
confidence, depending on converging evidence from many different
measures.
The logic of converging operations spells out, in formal detail,
what has been implied all along: if the study of consciousness is
to be put on a firm scientific basis, introspective self-reports
of phenomenal experience should be corroborated by objective
evidence of stimulus conditions (induction procedure), overt
behavior, or neural or other physiological correlates.
Stoyva and Kamiya's proposal was based on earlier theoretical work in perception, which confronts a problem similar to our problem: when considering subjects' reports of perceptual experience, how can we be sure that these reports are accurate? Garner, Hake, & Eriksen (1956) proposed that alternative explanations of subjects' perceptual self-reports could be ruled out by successive experiments. Therefore, the evidence for a particular perceptual effect did not depend on a particular measure, but rather by the convergence among several different measures.
The problem is even greater when we try to understand perception in infants and other pre-verbal children, or in animals, who can't talk to us at all. Proffitt and Bertenthal (1990) discussed the application of converging operations in the study of infant perception.
Campbell and Fiske (1959) proposed a similar solution to a similar problem in personality: how do we know that a person really possesses some trait like extraversion or neuroticism? Or even that such traits exist in the first place? They argued that personality variables were hypothetical constructs, which could be validated by a multitrait-multimethod matrix. In this method, investigators measure two or more personality traits (e.g., extraversion and neuroticism) by two or more methods (e.g., self-report and behavior). Given a large sample of subjects:
- Correlations across methods within a trait should be higher than correlations across methods between traits. This is known as trait variance.
- That is to say, the correlation between self-report and behavioral measures of extraversion should be greater than the correlation of either of these variables with self-report or behavioral measures of neuroticism.
- There may also be correlations between different traits measured by the same method. This is known as method variance.
- That is to say, the correlation between self-report measures of extraversion and neuroticism may also be significant, because of something (like a tendency to respond in a socially desirable way) that both measures share in common.
- If a trait is a valid construct, trait variance -- variance common to different measures of the same trait -- should be greater than method variance -- variance common to similar measures of different traits.
If you think about it, altered states of consciousness are also hypothetical constructs -- as, indeed, are normal states of consciousness
There are lots of different ways to get into a coma, but most involve some sort of traumatic brain injury (TBI), such as a gunshot wound to the head or a closed head injury (in which there is brain damage, but no external loss of blood).
Concussion is defined as a temporary disturbance of
consciousness resulting from a closed head injury.
Concussions can be "graded" according to their
severity. One such scheme, promoted by the American
Academy of Neurology, goes like this:
In mild concussion, consciousness is only impaired, as in the "ding" all-too-commonly experienced by football players.
In a provocative study, Yarnell and Lynch (1973) studied college football players who suffered either concussion or broken limbs over the course of 18 games. As soon as possible after the injury, these investigators presented the players with a series of informal tests. For example, they were asked if they remembered receiving a medical examination on the field; if they remembered their injury, and what play was in progress. Although all of the concussed players were disoriented immediately after their injury, none of the players actually lost consciousness. Nevertheless, they lost conscious recollection within minutes of their injury -- sometimes with a lucid interval, in which they could remember, before the amnesia set in.
At the very lowest end of the continuum of consciousness is coma,
(a state of complete unconsciousness in which the patient is
unresponsive even to the most vigorous and painful
stimulation):
Stupor is a state of suppressed consciousness in which only very vigorous stimulation elicits a response from the patient.
Clinically, coma is assessed by means of the Glasgow Coma Scale (GCS), which quantifies the patient's "best" response to a number of different stimuli (Teasdale & Jennett, 1974):
|
Best Eye Response: |
Best Verbal Response: | Best Motor Response |
| 1 -
No eye opening 2 - Eye opening to pain 3 - Eye opening to verbal command 4 - Eyes open spontaneously |
1 - No verbal response 2 - Incomprehensible sounds 3 - Inappropriate words 4 - Confused 5 - Orientated (sic) |
1 - No motor
response 2 - Extension to pain 3 - Flexion to pain 4 - Withdrawal from pain 5 - Localizing pain 6 - Obeys commands |
 The GCS is very popular, but it has
some problems -- mainly, that it requires an assessment of
a verbal response, when many brain-injured patients have
been intubated, and thus cannot speak. Accordingly,
a group of neurologists at the Mayo Clinic have proposed a
new scale, known as the FOUR score -- for Full Outline of
UnResponsiveness (Wijdicks et al., 2005). The FOUR
score assesses eye and motor responses, much as the GCS
does; but instead of a verbal response, it assesses
respiration and brainstem reflexes. The FOUR scale
can be administered to nonverbal patients, and it also
appears to make finer distinctions among patients with the
lowest scores on the GCS.
The GCS is very popular, but it has
some problems -- mainly, that it requires an assessment of
a verbal response, when many brain-injured patients have
been intubated, and thus cannot speak. Accordingly,
a group of neurologists at the Mayo Clinic have proposed a
new scale, known as the FOUR score -- for Full Outline of
UnResponsiveness (Wijdicks et al., 2005). The FOUR
score assesses eye and motor responses, much as the GCS
does; but instead of a verbal response, it assesses
respiration and brainstem reflexes. The FOUR scale
can be administered to nonverbal patients, and it also
appears to make finer distinctions among patients with the
lowest scores on the GCS.
Coma is often followed by a persistent vegetative
state, in which the patients' bodily functions are
normal but there is no evidence of
consciousness. While the patient's eyes are
open, giving the appearance of vigilance, and may even
follow motion around the room, the patient shows no
differential behavioral response to meaningful
stimulation. PVS is best described as "wakefulness
without consciousness":
But do PVS patients go through actual
sleep cycles, alternating between stages of Rapid Eye
Movement (REM) and Slow-Wave Sleep (SWS)? There have been
remarkably few psychophysiological studies of sleep in
comatose or vegetative patients (Cologan et al., Sleep
Medicine Reviews 2009). Based on the little evidence
available:
However, the absence of REM activity has been reported in some vegetative patients. This suggests that the diagnosis of PVS vs. coma could be improved by the use of polysomnography to actually document sleep activity in these patients -- as opposed to a reliance on behavioral signs such as the periodic closing and opening of the eyes. Patients who cycle between REM and SWS would be diagnosed as vegetative; those who do not would be diagnosed as comatose. This is especially the case if, as appears to be the case from the limited evidence, signs of normal sleep patterns appear to be associated with better prognosis for recovery. For more details about polysomnography, see the lecture supplements on Sleep and Dreams.
PVS was first described by Jennett and Plum in 1972. In
2005, it was estimated that there were approximately
10-15,000 patients diagnosed with PVS in the United
States.
PVS also goes by the somewhat less daunting label unresponsive
wakefulness syndrome, which has the advantage of not
implying that the patient is a "vegetable".
 PVS
PVS  is relatively
rare in absolute terms, and is most likely to occur within 1
month of the patient's head injury. Recovery from the
PVS is most likely to occur within 6 months of onset, and
PVS patients almost never recover after three months --at
which time the vegetative state can truly be called persistent. In
1994, a review of over 700 cases of PVS revealed not a
single instance of recovery after two years in the state.
is relatively
rare in absolute terms, and is most likely to occur within 1
month of the patient's head injury. Recovery from the
PVS is most likely to occur within 6 months of onset, and
PVS patients almost never recover after three months --at
which time the vegetative state can truly be called persistent. In
1994, a review of over 700 cases of PVS revealed not a
single instance of recovery after two years in the state.
 Still,
recoveries are possible even after moderately prolonged
periods of time. In 2002, a woman in Tustin,
California fell into a coma one day after giving birth, and
10 minutes following surgery for a brain tumor. After
one year, she opened her eyes, turned toward her mother, and
smiled. Now she is able to lift her arms and hold her
child. However, she cannot smile, walk, or talk --
instead, she communicates by rolling her eyes (West
County Times, 04/07/03). But anecdotal reports
of "miracle recoveries", after years in coma or PVS, are
largely unverified.
Still,
recoveries are possible even after moderately prolonged
periods of time. In 2002, a woman in Tustin,
California fell into a coma one day after giving birth, and
10 minutes following surgery for a brain tumor. After
one year, she opened her eyes, turned toward her mother, and
smiled. Now she is able to lift her arms and hold her
child. However, she cannot smile, walk, or talk --
instead, she communicates by rolling her eyes (West
County Times, 04/07/03). But anecdotal reports
of "miracle recoveries", after years in coma or PVS, are
largely unverified.
Note: A student pointed out an apparent contradiction in this case report: at the time of recovery, the patient smiled at her mother; but on later examination, she could neither smile nor talk. Here's my interpretation: the family was at the patient's bedside when the recovery occurred. There's no doubt that she turned her head, or made some other noticeable movement; but her expression may have been ambiguous, or even an involuntary facial expression, which was interpreted by her mother as a smile. Later careful testing, under more controlled conditions with more objective observers, did not confirm the patient's ability to smile voluntarily. But the recovery itself was obvious by the patient's ability to interact with her child and communicate via eye movements.
Recently, yet a third neurological syndrome has been
described, the minimally conscious state
(Giacino, 2002; see also "What if There is Something Going
On in There?" by Carl Zimmer, New York Times Magazine,
09/28/03). This is a state of "partial, inconsistent
consciousness":
PVS was first described by Giacino and Schiff in
2002. In 2005, it was estimated that there may have
been as many as 100,000 patients with MCS in the United
States -- some misdiagnosed as in coma or PVS. It
seems that recovery from coma progresses through PVS to MCS,
and -- if the patient is lucky -- to the recovery of fuller
consciousness.
So, in the final analysis, all the medical questions hinge on whether Ms. Schiavo is, in fact, conscious to any degree.
It would be nice to think that formal neurological and neuroscientific testing would have helped resolve this issue. In fact, previous testing had indicated that Ms. Schiavo's EEG record was flat, indicating no cortical activity, and a CT scan indicated that about 95% of her brain tissue had been replaced by fluid. There are standards for distinguishing between PVS and MCS, based mostly on careful observations of the patient's response to environmental stimuli; in principle, these could be developed into formal laboratory tests of the sort used to diagnose other forms of medical illness. But note that MCS was only described for the first time in 2002. Before that, the only diagnostic choice was PVS. Nevertheless, none of these formal tests had been performed during the later stages of the case. Perhaps the court should have ordered a new round of testing, conducted by an impartial expert, to determine the proper diagnosis. But it is not clear that even confirmation of MCS, as opposed to PVS, would have changed the legal situation -- because the essence of Mr. Schiavo's argument is that Ms. Schiavo had expressed a desire not to be kept alive artificially -- presumably, even if she were in fact fully conscious.
A New York Times commentary on the Schiavo case was headlined, "Did Descartes Doom Terri Schiavo?" (article by John Leland, 03/27/05). The writer argued that while Aristotle had held that "existence itself to be inviolable", Descartes "defined human life not as biological existence -- which might be an inviolable gift from God -- but as consciousness, about which people can make judgments." But it doesn't seem that the Schiavo case is really about whether some lives are worth living, or whether the value of a human life can be quantified. To be sure, there is a legitimate debate about Ms. Schiavo's true wishes -- but legally, patients have a right -- affirmed in a Supreme Court decision -- to make this decision for themselves, and to refuse treatment, and even Catholic doctrine permits them to do so. Rather, the question in this case is whether Ms. Schiavo, lacking a brain, lacks consciousness as well; and so it hinges on questions about how much brain she has, and how much brain is required for consciousness.
In fact, the Cartesian perspective seems to cut both ways. True, Descartes argues that consciousness is a uniquely human characteristic; without consciousness, a human being is just another animal -- an animal that does not, in Descartes' view, experience pain, and which presumably may be deprived of life at will. But on the other hand, consciousness for Descartes is not just about the mind. For Descartes as a devout Catholic, consciousness was the mark of a person's immortal soul. And for Descartes as a substance dualist, the soul/mind was immaterial, not part of the body, and survived the body after death. In the final analysis, for Descartes, it doesn't matter whether a person has a functioning brain, because the brain has nothing to do with either soul or mind.
In a commentary written and published before Ms. Schiavo's death, Hendrik Hertzberg wrote, "The body lived; the mind died.... Terri Schiavo's life, as distinct from the life of her unsentient organs, ended fifteen years ago". Nevertheless, he continued, "On a human level, it was hard to see what concrete harm there could be in indulging her family's wish to keep her body alive, its care presumably underwritten by the hospice and the family's supporters" ("Matters of Life", New Yorker, 04/04/05). Here again, we see how the argument about mind and body cuts both ways. If Ms. Schiavo no longer had a mind, because she no longer had a brain, then it is possible to argue that her husband, or her parents, could do what he, or they, wanted with her body. But that doesn't seem right either. Do we really want cases like this to degenerate into a battle over custody -- that is, in essence, a battle over property rights? But time and again, the courts determined that her own wishes, expressed when she had a brain, and thus a mind, controlled the disposition of the case. If only she had expressed them in writing, in front of witnesses. Then she (or, at least, her memory), and they, and us, would have been spared the spectacle.
Actually, history repeated itself in 2009, with Eluana Englaro, an Italian woman who had been in a persistent vegetative state since 1992. Her father, Beppino Englaro, had petitioned to remove her feeding tube, reflecting what he said was her frequently expressed wish before she was injured in an automobile accident. Despite the opposition of the Catholic Church, several court decisions, including one by the Constitutional Court, had allowed the feeding tube to be removed. At the last minute, the conservative government of Prime Minister Silvio Berlusconi issued an emergency decree to prevent the removal, but President Giorgio Napolitano refused to sign it, instigating a constitutional crisis. Berlusconi, in turn, drafted a bill for the Italian Parliament, where his coalition has a substantial majority. The feeding tube was removed, and Ms. Englaro died on February 9, 2009, before Parliament could take action ("Italy Moves to Keep Alive a Woman in a Coma" by Rachel Donadio, New York Times, 02/07/2009).
Coma and PVS are to be contrasted with the "locked in" syndrome, where the person is fully conscious but cannot communicate beyond eye signals.
Locked-in syndrome was made
famous by Awakenings, an early book about
Parkinson's disease by Oliver Sacks, subsequently made
into a film starring Robin Williams (who captured Sacks'
demeanor perfectly). And also by The Diving Bell
and the Butterfly, a book (and subsequent movie) by
Jean-Dominique Bauby, former editor of a French fashion
magazine, recounting his own experience of locked-in
syndrome, following a massive stroke at age 42.
"Locked-in" patients have
severe motor difficulties, which is why they're called
"locked-in". But by every standard they are
consciously aware of both the external environment and
their internal states.
Coma-Related Conditions Compared
|
||||
Coma |
PVS |
Locked-In Syndrome |
Brain Death |
|
|
Absent |
Absent |
Present |
Absent |
|
Absent |
Intact |
Intact |
Absent |
|
No Purposeful Movement |
No Purposeful Movement |
Quadriplegia
with Preserved Eye Movement |
None
or Only Spinal Reflexes |
|
No |
No |
Yes |
No |
|
Depressed |
Normal |
Normal |
Absent |
|
Delta or Theta |
Delta
or Theta, sometimes slow Alpha |
Normal |
EEG "Silence" |
|
Reduced by > 50% |
Reduced by > 50% |
Minimal Reduction |
Absent |
|
Recovery,
PVS, or Death, usually within 2-4 Weeks |
Depends on cause |
Recovery unlikely |
No Recovery |
Coma is
primarily associated with damage either to the
posterior portion of the upper brain stem -- the
area known as the reticular formation (including the
periaqueductal gray and the parabrachial nucleus), which
serves to maintain general levels of cortical arousal
and alertness.
At first thought, it
would seem that stupor, PVS, and MCS are associated with
damage to these same areas, though presumably less
severe than in the case of coma. Actually, PVS is commonly associated with
damage to the thalamus, as opposed to the
brainstem. The thalamic damage impairs awareness,
while the spared brainstem continues to generate the
sleep-wake cycle. Because the
thalamus serves as a general sensory relay center,
presumably the thalamic damage prevents incoming
sensory impulses from being processed by the
cortex. PVS is more common following
anoxia, which affects the brain as a whole, than
following a traumatic head injury, whose affects may be
more localized.
The pattern of brain damage in the
"locked-in" syndrome differs from that observed in
coma. Here the damage is in the pons and
upper anterior portion of the brain stem, and
excludes the reticular formation. Because the
reticular formation and thalamus are both spared,
consciousness and the sleep-wake cycle are also
spared.
So exactly how do locked-in patients
get locked in? Most of the efferent pathways that
connect the brain to the cranial and spinal nerves pass
through the pons. So, if the pons is destroyed,
efferent signals can't get where they're supposed to go,
and the person is effectively paralyzed. But, it
turns out that the damage to the pons is confined to
areas below where the trigeminal nerve (V cranial nerve)
enters the brainstem. As a result, the oculomotor
nerve (cranial nerve III) and the trochlear nerve
(cranial nerve IV) nerves are unaffected, sparing
voluntary movements of the eyes and eyelids. It
was by this means that Jean-Dominique Bauby was able to
write The Diving Bell and the Butterfly.
Because his right eye had been sewn shut to prevent
infection, he "dictated", spelling out each letter
individually by blinking his eyes when his scribe
pointed to the correct letter on a display.
The different pathologies in coma and
the locked-in syndrome underscore the role of the
reticular formation in maintaining conscious alertness
and wakefulness. In 1949, Moruzzi and Magoun
described the reticular activating system based
on studies of lesions and stimulation in this area in
cats:
Damasio argues that the
reticular activating system is not confined to the
reticular formation, but also extends into the
thalamus. Moreover, it appears that different
nuclei within the reticular formation may have different
functions with respect to consciousness:
Damasio argues for the existence of an unconscious proto-self, associated with the reticular formation, which monitors the physical condition of the organism. This proto-self is spared even in states, such as coma and the "locked-in" syndrome, where the consciousness associated with the core and autobiographical selves is abolished. It is this proto-self that, presumably, maintains the vegetative functions that are preserved even when consciousness is abolished in coma.
However, it is unclear what Damasio's concept adds to the familiar concept of homeostatic regulation, the negative feedback system(s) by which organisms monitor and maintain important physiological parameters (body temperature, fluid levels, nutrients) within the critical ranges necessary to preserve life. And we know that the hypothalamus -- a structure located in the subcortical limbic system, and not generally associated with the reticular activating system -- plays a major role in thermoregulation and perhaps eating as well (drinking appears to be regulated by one or more circumventricular organs embedded in the walls of the cerebral ventricles).
In a sense, homeostatic regulation is self-regulation, and self-regulation implies a self -- if only the proto-self of Damasio. The proto-self may be the anlagen, or forerunner, of the more cognitive core and autobiographical selves, which is what Damasio seems to be arguing. But it's also the case that thermostats engage in homeostatic regulation, and nobody (except maybe David Chalmers) argues that thermostats have a self, much less consciousness. Better, I think, to leave homeostatic regulation out of the picture of consciousness -- unless departures from homeostasis are associated with the actual conscious experiences -- qualia -- of warmth, cold, thirst, and hunger.
Laborious as it might be, it's clear how to communicate with patients suffering from the locked-in syndrome. In both coma and PVS, but especially in the latter, the possibility has been raised that the patients are aware of their surroundings, even if they are not responsive to them (this was an issue in the Terry Schiavo case). In principle, mental activity of this sort could be assessed by the same sorts of priming techniques employed to document implicit memory and perception in general anesthesia.
An experiment by Turkstra (1995) represents a pioneering effort in this direction. Her patients were diagnosed with PVS (patients in acute PVS, for less than 3 months; patients in chronic PVS, for more than 1 year; and patients who had recovered from PVS, as well as controls).
 In her
experiment, Turkstra recorded physiological responses
(galvanic skin potential, a measure of the electrical
properties of the skin) to acoustic startle stimuli,
orientation and habituation, and response to famous vs.
non-famous faces and to intelligible vs. unintelligible
written commands. Although some PVS patients --
particularly, those in an acute state -- showed evidence
of startle, orientation, and habituation.
In her
experiment, Turkstra recorded physiological responses
(galvanic skin potential, a measure of the electrical
properties of the skin) to acoustic startle stimuli,
orientation and habituation, and response to famous vs.
non-famous faces and to intelligible vs. unintelligible
written commands. Although some PVS patients --
particularly, those in an acute state -- showed evidence
of startle, orientation, and habituation.
 However,
there was no evidence of appropriate response to the
faces or commands.
However,
there was no evidence of appropriate response to the
faces or commands.
A follow-up study showed that those PVS patients with preserved startle (etc.) were more likely to recover from the PVS (this was true for the acute group, but not the chronic group). Unfortunately, Turkstra did not determine whether these recovered patients had any memory (implicit or explicit) for the original test stimuli. Still, the finding does have some implications for predicting patients' response to rehabilitation efforts.
It has also been discovered that some PVS patients can show some degree of learning. Bekinschtein et al. (2009) presented PVS patients with a tone followed by a puff of air to the cornea. The air puff normally elicits a reflexive eyeblink, and after enough trials, neurologically intact patients will show a conditioned eyeblink response to the tone as well. Adequately anesthetized patients do not show the conditioned eyeblink response, but some PVS patients do -- and whether they can learn predicted the extent of their recovery, assessed one year later.
Similar studies quickly followed the description of the minimally conscious state by Giacino et al. (2002). As described earlier, MCS is generally diagnosed clinically by observing the patient's behavioral responses to various stimuli. However, various sorts of brain-imaging techniques can be employed to detect mental activity in these patients (and, of course, patients who are comatose or vegetative).
For example, Schiff et al. (2005) reported a pioneering brain-imaging study of 2 patients in the minimally conscious state, one of whom also had damage to the left temporal lobe, including the language areas -- which, as we'll see, compromised the experiment somewhat. But in clinical research, you don't always get to pick your patients.
 Light tactile
stimulation of the patients' hands led to activation in
the primary somatosensory cortex, and particularly in the
"anatomic hand area".
Light tactile
stimulation of the patients' hands led to activation in
the primary somatosensory cortex, and particularly in the
"anatomic hand area".
 Auditory
Auditory  narratives of familiar events, read in
a familiar voice, led to activation of language centers
associated with the recognition of speech. These
areas were not activated by the same passages presented in
reversed speech, and thus devoid of semantic
content. Unfortunately, one patient had suffered
damage in Wernicke's area, and produced negative
results. The other patient, whose language areas
were intact, showed significant but "reduced engagement"
of language centers by speech.
narratives of familiar events, read in
a familiar voice, led to activation of language centers
associated with the recognition of speech. These
areas were not activated by the same passages presented in
reversed speech, and thus devoid of semantic
content. Unfortunately, one patient had suffered
damage in Wernicke's area, and produced negative
results. The other patient, whose language areas
were intact, showed significant but "reduced engagement"
of language centers by speech.
Another
study, by Perrin et al. (2006), examined event-related
potentials generated in response to auditory stimuli
such as the patients' own first names vs. another's
first name. Perrin's focus was on patients in MCS,
but his study also included patients in the persistent
vegetative state and the locked-in syndrome, as well as
age-matched, neurologically intact, controls.
Perrin's experiment focused on four well-studied
"cognitive" components of the ERP: N1, P1, N2, and P3.
The results were complex, but let's focus on P3, otherwise known as P300, which generally is responsive to unexpected, or surprising, stimuli. If an experimenter plays a string of high-pitched "beeps" followed by a low-pitched "boop", subjects will show an enhanced P3 wave to the novel, unexpected stimulus. Similarly, subjects will show an enhanced P3 to their own names -- much as in Cherry's study of the cocktail party phenomenon.
The control
subjects showed a very large P3 response to their own
names. Patients in the minimally conscious state
or the locked-in syndrome also showed a substantial P3,
though somewhat diminished in amplitude. Patients
in the persistent vegetative state showed considerably
smaller P3 responses. This is pretty much the way
the predictions would go, but note that, with respect to
some of the other components, PVS patients showed more
response than MCS or locked-in patients, or even
controls! You can't pick your subjects, and you
can't pick your results, either, and these complications
warrant further investigation.
Returning to
P3, however, setting aside the question of the amplitude
of P3, let's just look at whether the patients displayed
any evidence of P3 at all. Here, the
results were more straightforward. Of course, all
of the control patients showed a P3. So did all of
the locked-in patients -- which makes sense, because
there's no question that these patients are
conscious. But so did all the MCS patients, which
is consistent with the proposition that they are at
least minimally conscious. But so did a
majority of the PVS patients, which raises the question
of whether at least they, too, might be at least
minimally conscious.
On the other hand, P3 is also ambiguous. Yes, it represents an orienting response to an unexpected stimuli, but such orienting responses can be displayed even by organisms with extremely simple nervous systems -- organisms that we would not ordinarily characterize as conscious. Even in human subjects, P3 can occur in response to subliminal stimulation, of which the subject is unaware. P3 may also reflect an automatic, and thus unconscious, component of speech comprehension. What we really need is unambiguous evidence of conscious mental activity in coma, or PVS, or MCS.
One
possibility was suggested by a case study by a
multinational group of British and Belgian
investigators, with a 23-year-old woman who suffered
traumatic brain injury following an automobile accident,
and who had been diagnosed with PVS (Owen et al., 2006,
2007). She had been unresponsive for five months,
though she also displayed the usual sorts of sleep
cycles. Using fMRI, Schiff et al. (2002) had shown
that she displayed increased activation in her
left-hemisphere speech and language centers when
presented with speech sounds versus noise, and also with
sentences containing ambiguous words (e.g., The
creak came from a beam in the ceiling).
Again, as with P3, such evidence is equivocal with
respect to consciousness. A better test
came from a second fMRI study (Owen et al., 2006), in
which the patient was instructed to imagine either
playing tennis (e.g., swinging a racket) or walking
through her house. In response, the patient showed
increased activation in the supplementary motor area
(where voluntary motor responses are prepared for
execution by the primary motor cortex) and the
parahippocampal gyrus (an area of the medial temporal
lobe known to be involved in spatial processing).
This pattern of brain activity, reflecting the cortical
processing specific to the understanding and execution
of a request for voluntary motor behavior, certainly
qualifies as evidence of consciousness -- in both its
monitoring and controlling aspects.
More
recently, this same group of investigators have gone
beyond their earlier single-case demonstration
experiment study to test a large sample of 54 patients
-- 23 with PVS, and 31 in the MCS -- as well as 16
healthy controls (Monti et al., 2010). Of these 54
patients, five showed task-specific differential
response to the instructions, activating the
supplemental motor cortex during tennis imagery, and the
parahippocampal gyrus during spatial imagery.
That's a very small minority of these patients -- but
it's something. Interestingly, this group of five
consisted of 4 PVS patients, and only one MCS
patient. One would have thought, and certainly the
investigators expected, that the ratio would be the
other way around.
 Here's a detailed
comparison of the five responsive patients, following
the instruction to imagine playing tennis (Owen, 2013).
Patient 5 is the patient studied by Owen et al. (2006,
2007). Patients 1-4 are the 4 PVS patients from Monti et
al. (2010). The same areas of the cortex were activated
in the patients as in neurologically intact controls.
Here's a detailed
comparison of the five responsive patients, following
the instruction to imagine playing tennis (Owen, 2013).
Patient 5 is the patient studied by Owen et al. (2006,
2007). Patients 1-4 are the 4 PVS patients from Monti et
al. (2010). The same areas of the cortex were activated
in the patients as in neurologically intact controls.
 Cruse and his
colleagues performed a similar study measuring brain
activity with EEG rather than fMRI (Lancet, 2011;
Neurology 2012). Three groups of subjects
-- 16 PVS patients, 23 MCS patients, and 12
neurologically intact controls -- were asked to imagine
squeezing their right hand, or wiggling their left toe,
whenever they heard a signal. A statistical
algorithm was then used to classify EEG activity in the
premotor cortex, focusing on the "hand" and "toe" areas
of the motor homunculus; the brain responses of 9/12
controls were decoded successfully. Decoding was
similarly successful for 3/16 PVS patients (19%) and
5/23 MCS patients (22%). It is important to note,
however, that this index of consciousness was apparent
in only a minority of patients -- roughly 20%.
Cruse and his
colleagues performed a similar study measuring brain
activity with EEG rather than fMRI (Lancet, 2011;
Neurology 2012). Three groups of subjects
-- 16 PVS patients, 23 MCS patients, and 12
neurologically intact controls -- were asked to imagine
squeezing their right hand, or wiggling their left toe,
whenever they heard a signal. A statistical
algorithm was then used to classify EEG activity in the
premotor cortex, focusing on the "hand" and "toe" areas
of the motor homunculus; the brain responses of 9/12
controls were decoded successfully. Decoding was
similarly successful for 3/16 PVS patients (19%) and
5/23 MCS patients (22%). It is important to note,
however, that this index of consciousness was apparent
in only a minority of patients -- roughly 20%.
Note, however, that in the Cruise et al. studies,
roughly the same proportion of PVS and MCS patients
responded positively to the commands. But almost by
definition, we would expect to see more
differential responsiveness in the MCS patients --
precisely because they are supposed to be at least minimally
conscious, compared to the PVS patients who are
presumably unconscious, and operating on reflexes at
best.
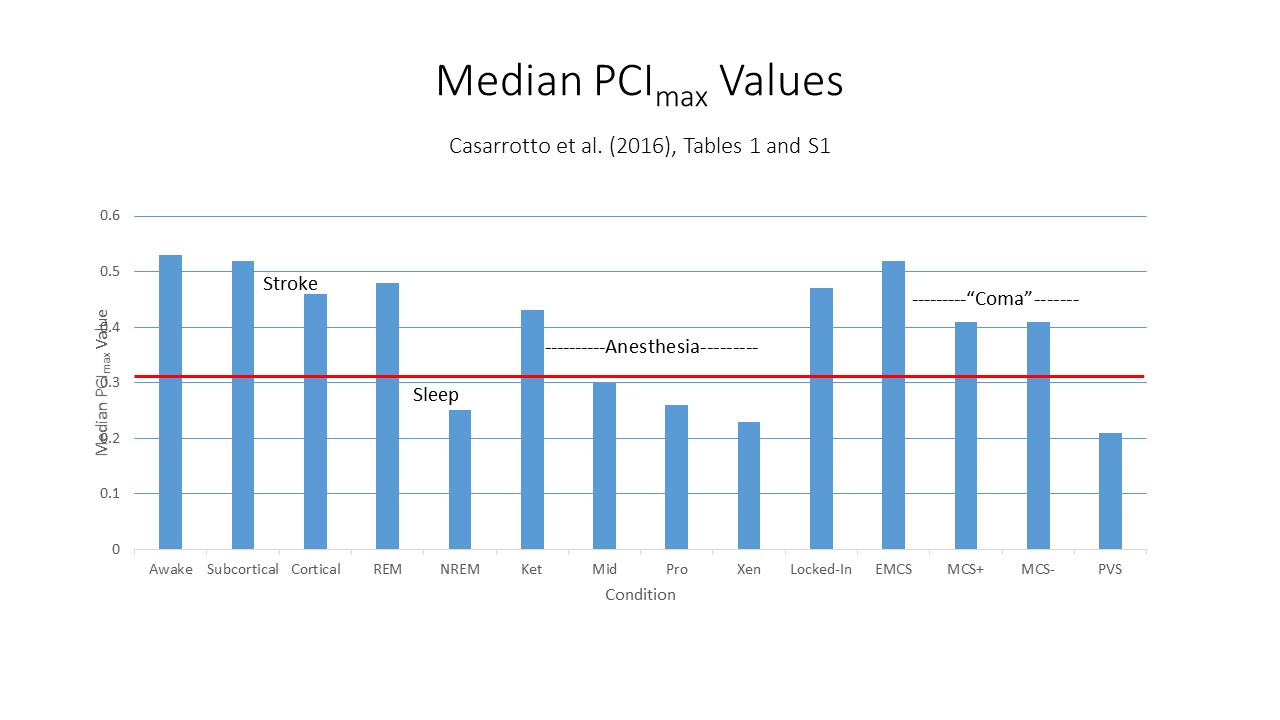 Another
approach to differentiating PVS from MCS relies on the
PCI index of consciousness discussed in the lectures on
Mind and Body. Recall that Casarotto et al.
(2016) performed a "benchmarking" study which
established a value of PCI* = .31 for distinguishing
between subjects who are conscious and those who are
not. These investigators also employed this index
in a sample of patients with PVS or MCS. The MCS
patients were further divided into two groups, MCS+ and
MCS-, depending on their scores on the Coma Recovery
Scale-Revised (CRS-R); there was also a group of former
MCS patients who had "emerged" from their coma.
The EMCS patients had median PCImax scores
comparable to those of waking subjects with no brain
damage, .52 vs. .53. All the MCS+ and MCS-
subjects also had PCImax scores exceeding the threshold
PCI* value, medians = .41 and .38,
respectively. The median score for the PVS
patients (.21)
did not cross
this threshold; however, 9 individual patients (out of
43, or 21%) had PCImax scores that did exceed the
threshold. These patients would be candidates for
further investigation, and might qualify for a diagnosis
of MCS instead of PVS.
Another
approach to differentiating PVS from MCS relies on the
PCI index of consciousness discussed in the lectures on
Mind and Body. Recall that Casarotto et al.
(2016) performed a "benchmarking" study which
established a value of PCI* = .31 for distinguishing
between subjects who are conscious and those who are
not. These investigators also employed this index
in a sample of patients with PVS or MCS. The MCS
patients were further divided into two groups, MCS+ and
MCS-, depending on their scores on the Coma Recovery
Scale-Revised (CRS-R); there was also a group of former
MCS patients who had "emerged" from their coma.
The EMCS patients had median PCImax scores
comparable to those of waking subjects with no brain
damage, .52 vs. .53. All the MCS+ and MCS-
subjects also had PCImax scores exceeding the threshold
PCI* value, medians = .41 and .38,
respectively. The median score for the PVS
patients (.21)
did not cross
this threshold; however, 9 individual patients (out of
43, or 21%) had PCImax scores that did exceed the
threshold. These patients would be candidates for
further investigation, and might qualify for a diagnosis
of MCS instead of PVS.
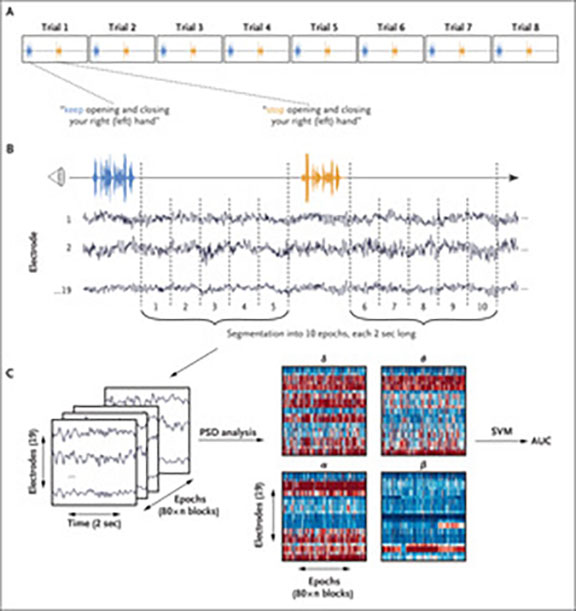 All
All
 of
the studies described so far have concerned "chronic"
patients, who have been in a coma or PVS for a
substantial period of time. But it is also
possible to perform such studies with more "acute"
patients, whose condition had a more recent onset.
Just such a study was reported by Claassen, Rokaut, and
their colleagues (Claassen et al., NEJM
06/27/2019), employing a large sample of 104 patients
with acute brain injury due to heart attack, cerebral
hemorrhage, traumatic brain injury, and the like. Most
of these patients were diagnosed with coma or PVS; some
were diagnosed with "MCS-minus". Responsiveness to
commands was assessed via EEG, with a large array of
electrodes attached to the skull. The patients
were then instructed, over several trials, to "keep
opening and closing" or "stop opening and closing" their
hands (of course, they weren't able to do this overtly,
because their condition effectively rendered them
paralyzed). Employing machine learning, the
investigators first identified an algorithm that could
distinguish between the EEG responses to these commands
in neurologically intact subjects. They then
applied this algorithm to the brain-damaged patients,
who were tested within about a week of admission.
of
the studies described so far have concerned "chronic"
patients, who have been in a coma or PVS for a
substantial period of time. But it is also
possible to perform such studies with more "acute"
patients, whose condition had a more recent onset.
Just such a study was reported by Claassen, Rokaut, and
their colleagues (Claassen et al., NEJM
06/27/2019), employing a large sample of 104 patients
with acute brain injury due to heart attack, cerebral
hemorrhage, traumatic brain injury, and the like. Most
of these patients were diagnosed with coma or PVS; some
were diagnosed with "MCS-minus". Responsiveness to
commands was assessed via EEG, with a large array of
electrodes attached to the skull. The patients
were then instructed, over several trials, to "keep
opening and closing" or "stop opening and closing" their
hands (of course, they weren't able to do this overtly,
because their condition effectively rendered them
paralyzed). Employing machine learning, the
investigators first identified an algorithm that could
distinguish between the EEG responses to these commands
in neurologically intact subjects. They then
applied this algorithm to the brain-damaged patients,
who were tested within about a week of admission.
Now, we don't know whether the CBD patients
were actually aware of the commands at the time they were
tested: apparently the researchers didn't think to ask
them. And it's possible that, with such simple, probably
automatized behaviors, that the subjects could have responded
without conscious awareness of what they were doing.
Still, the Claassen et al. study adds to the evidence that some
minimal degree of consciousness may be spared even in comatose
patients. But only a minority show CBD -- and even
then, some CBD patients never recover fully.
Based on the finding of differential
responsiveness in at least some PVS and MCS patients,
and perhaps inspired by Jean-Dominique Baudry,
researchers have been interested in investigating the
use of EEG and fMRI to establish two-way communication
with patients in PVS or MCS. The general idea is
to associate specific motor images (e.g., of playing
tennis or walking around a house) with particular
responses (e.g., yes or no) to questions.
In
 the Monti et al.
(2010) study, only one of the five
patients (out of a total of 54 patients, remember) was
able to answer questions in this manner: 5 out of 5
correct, in fact -- further evidence of conscious
awareness and control on the part of this patient, at
least. In case there were any doubt, plots of the
time course of activation show clearly that this patient
responded quickly to each question, activating the
"tennis" or the spatial "navigation" task, with the
activation dissipating when the patient was instructed
to "relax". The case is all the more remarkable,
perhaps, for the fact that this patient had been in the
PVS for five years when tested.
the Monti et al.
(2010) study, only one of the five
patients (out of a total of 54 patients, remember) was
able to answer questions in this manner: 5 out of 5
correct, in fact -- further evidence of conscious
awareness and control on the part of this patient, at
least. In case there were any doubt, plots of the
time course of activation show clearly that this patient
responded quickly to each question, activating the
"tennis" or the spatial "navigation" task, with the
activation dissipating when the patient was instructed
to "relax". The case is all the more remarkable,
perhaps, for the fact that this patient had been in the
PVS for five years when tested.
So beyond using brain-imaging techniques to improve the differential diagnosis of PVS and MCS, these same techniques may be useful in establishing communication with these patients. EEG is, of course, much easier to use than fMRI, and considerably cheaper. Perhaps, with this means of establishing communication with patients, it will be easier for families to make "end of life" decisions -- by asking the patients themselves what they want.
But before any of these techniques are used to communicate with ostensibly comatose patients, we have to be sure that the signals recorded in the EEG mean what we think they mean. In that respect, Goldfine et al. (Lancet 2012) criticized the methods used by Cruse et al. They subsequently performed a re-analysis of the Cruse et al. (2011) PVS study (Goldfine et al., Lancet 2013). Using what they considered to be a more appropriate statistical algorithm, Goldfine et al. were able to successfully decode the EEG records of only 40% of the intact controls, and none of the PVS patients. They concluded, not that Cruse et al. were wrong, but that one has to be very careful with these methods, given what is at stake. Cruse et al. (2013) replied that their algorithm succeeded in detecting consciousness in 75% of normal controls, whereas the alternative proffered by Goldfine et al. missed almost half of these. So, while the Cruse method may be susceptible to false positives (i.e., detecting consciousness where there is none), the Goldfine method may be equally susceptible to false negatives (i.e., failing to detect is hardly better than no algorithm at all.
A remarkable feature of this exchange is that the authors of the Cruse and Goldfine papers are in fact colleagues, such that authors of opposing papers actually work together, and are supported by the same research grant.
"Coma Dreams"The jazz
pianist and composer Fred Hersch has written
an extended multimedia piece, "My Coma
Dreams", describing dreams that he experienced
during coma that lasted for two months,
brought on by a bout of pneumonia. But,
as Hersch himself noted, the dreams might have
occurred throughout his coma, or during the
three minutes -- or, for that matter, three seconds
-- before he awakened. The piece
premiered in 2011, and was reviewed by Ben
Ratliff in the New York Times
("Unconscious Lessons of a Jazzman",
05/10/2011). |
In addition to communicating with patients in VS MCS (and,
thereby, diagnosing MCS in the first place), it may also be
possible to spark (sorry) a revival from coma, at least
temporarily. Pioneering work by Yamamoto and Katayama (2005)
at Nihon University in Japan, and Schiff et al. (2007) at Cornell
Medical School, shows that bilateral deep brain stimulation (DBS)
of the intralaminar nuclei of the thalamus (ILN)
can lead to signs of cortical arousal that were not previously
present.
It's important to understand that none of these patients returned
to full functioning. Neither of these studies attempted to use DBS
to shift comatose patients into VS, or MCS -- though that, of
course, remains a possibility. Still, the success of these
early studies sheds light on the neural correlates of
consciousness. We know that activation in the reticular
formation passes through the thalamus to reach higher cortical
centers. Damage to either the reticular formation or the
thalamus causes coma. Perhaps these patients sustained
damage to the RF, so that this activation was shut off at the
beginning. In such a case, external stimulation of the
thalamus should restore some degree of conscious functioning, as
it apparently does. If the damage had been to the thalamus,
preventing activation arising from the reticular formation from
reaching higher cortical centers, it is not clear that DBS of the
thalamus would have had the same effect. In any event, DBS
underscores the role of the pathway from the reticular formation,
through the thalamus, to the cerebral cortex in maintaining
wakefulness.
For a popular account of the discovery of the Minimally Conscious State, and an exploration of the practical and ethical issues surrounding it, see Into the Gray Zone: A Neuroscientist Explores the Border Between Life and Death by Adrian Owen (2017).
So, with respect to the persistent vegetative state and the minimally conscious state, there is some evidence for conscious, intentional activity in these conditions, for some, but by no means for all, patients -- indeed, only a small minority of these patients show any evidence of conscious awareness. Studies using fMRI and other brain-imaging may well lead to the development of more refined diagnostic tools. For example, based on the extensive study of Monti et al. (2010), we would tend to doubt the clinical criteria for MCS. By any standard, more MCS than PVS patients should have shown evidence of conscious activity. On the other hand, their imagery task may well prove decisive in assessing consciousness in these patients, and in determining who, among PVS patients, really are at least "minimally conscious".
Based on the evidence from Monti et al., it seems doubtful that the imagery technique can serve as a means of communicating with "true" MCS patients. But it's something that is worth trying in patients who show at least minimal evidence of consciousness. When it works, the technique may prove useful for medical decision-making -- for example, consulting the patient about various medical decisions such as limitations on treatment or maintenance of life supports.
But once a patient has become comatose, or entered the persistent vegetative state, the responsibility for making these most difficult decisions will fall on the patient's family. All the more reason, I think, for everyone to give these conditions serious consideration, and consulting with family and physicians to create advance directives for medical decision-making. Terry Schiavo's husband said that she wouldn't have wanted to live in the persistent vegetative state; her parents thought otherwise, and in the subsequent court battle she became a political football. Everything would have gone differently had Ms. Schiavo made her intentions clear before she fell ill.
This page last
revised
06/28/2019.